Introduction
Heart sounds are vital auditory cues that provide significant insights into the heart’s health and functioning. Among these, the first heart sound, commonly referred to as S1, plays a crucial role. This sound, often described as the “lub” in the “lub-dub” sequence of a heartbeat, marks the beginning of ventricular systole, when the heart’s ventricles contract to pump blood into the arteries. In this comprehensive blog post, we will delve deep into the mechanics, significance, and clinical implications of the first heart sound.
Anatomy and Physiology of S1
Cardiac Anatomy Relevant to S1
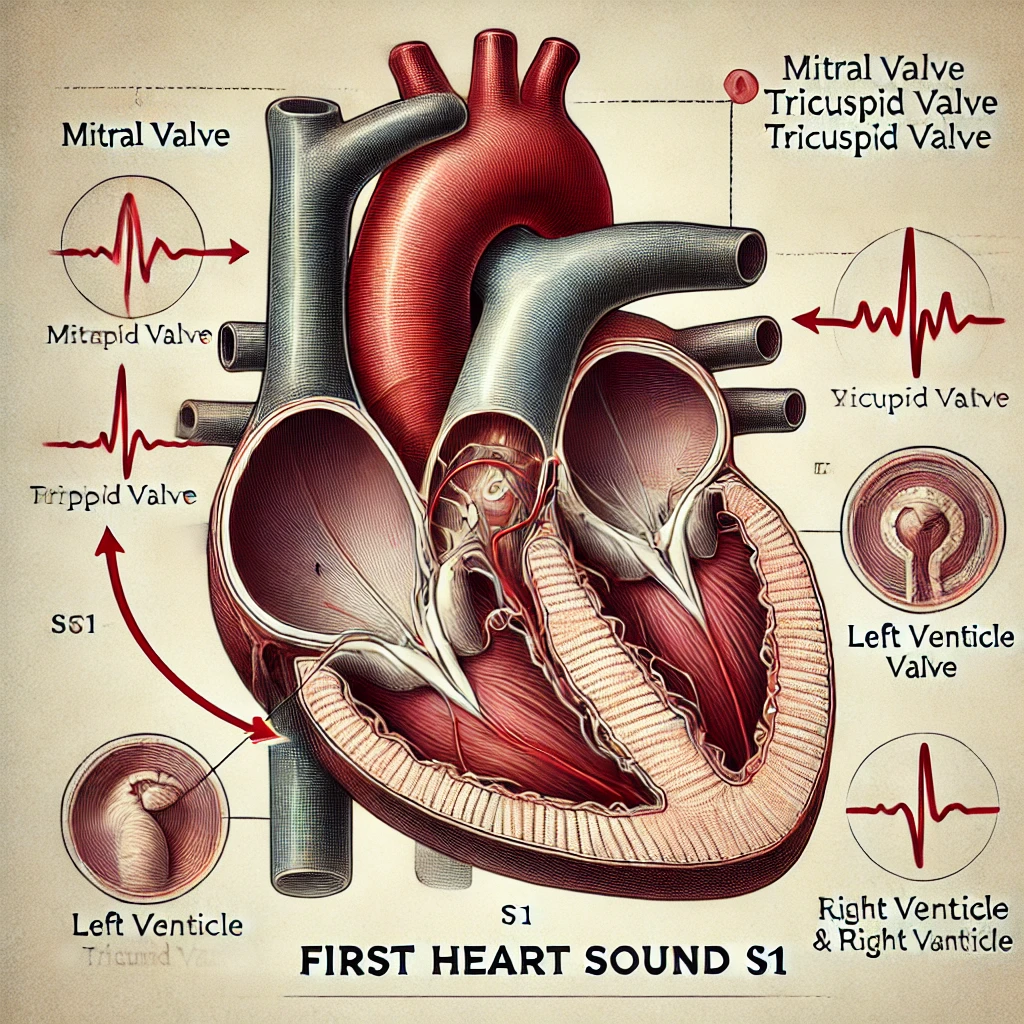
To understand the first heart sound, it’s essential to grasp the basic anatomy of the heart. The heart consists of four chambers: the right atrium, right ventricle, left atrium, and left ventricle. Blood flows through these chambers, guided by a set of valves that ensure unidirectional flow and prevent backflow.
- Atrioventricular Valves:
- Mitral Valve: Located between the left atrium and left ventricle.
- Tricuspid Valve: Located between the right atrium and right ventricle.
- Semilunar Valves:
- Aortic Valve: Situated between the left ventricle and the aorta.
- Pulmonic Valve: Positioned between the right ventricle and the pulmonary artery.
The first heart sound is primarily generated by the closure of the atrioventricular (AV) valves – the mitral and tricuspid valves. This event occurs at the onset of ventricular contraction (systole).
Physiology of S1
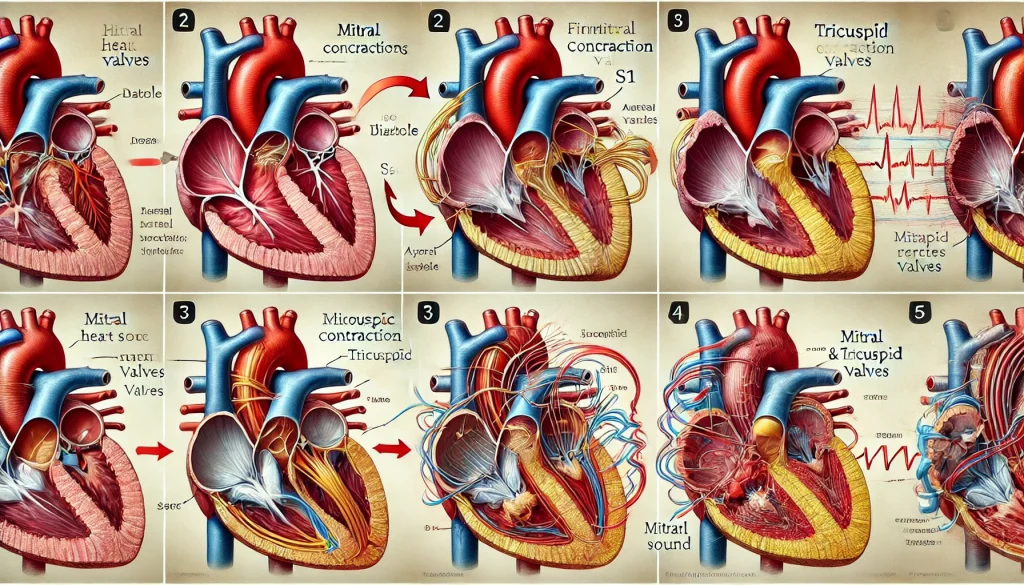
The first heart sound is produced due to the sudden closure of the mitral and tricuspid valves. Here’s a step-by-step breakdown of the process:
- Atrial Contraction: Blood fills the ventricles as the atria contract.
- Isovolumetric Contraction: The ventricles begin to contract with all valves closed, increasing pressure within the ventricles.
- Closure of AV Valves: As the ventricular pressure exceeds atrial pressure, the mitral and tricuspid valves snap shut. This sudden closure causes vibrations in the surrounding cardiac structures and blood, producing the S1 sound.
- Ventricular Ejection: Following the closure of the AV valves, the ventricular pressure rises further, eventually leading to the opening of the semilunar valves and the ejection of blood into the arteries.
Characteristics of the First Heart Sound
Acoustic Properties
The first heart sound is a complex, low-frequency sound that is best heard over the apex of the heart, typically located at the fifth intercostal space at the midclavicular line. It is a relatively long sound compared to the second heart sound (S2), and it has two major components:
- M1 (Mitral Component): The closure of the mitral valve generates the M1 sound. This component is louder and occurs slightly earlier than the tricuspid component due to the higher pressures in the left heart.
- T1 (Tricuspid Component): The closure of the tricuspid valve generates the T1 sound. This component is softer and occurs just after the mitral component.
Timing in the Cardiac Cycle
The S1 sound marks the beginning of systole and is synchronous with the upstroke of the carotid pulse. It occurs just after the QRS complex on an electrocardiogram (ECG), which represents ventricular depolarization.
Factors Influencing the Intensity of S1
Several factors can affect the intensity of the first heart sound:
- Distance Between Valve Leaflets and Ventricular Wall: A larger distance can result in a louder S1.
- Ventricular Contraction Force: Stronger contractions produce a louder S1.
- Valve Mobility and Thickness: Stiff or calcified valves may produce a softer S1.
- Heart Rate: A faster heart rate can increase the intensity of S1 due to reduced diastolic filling time and increased atrial contraction force.
Clinical Significance of S1
Normal Variations
The intensity and characteristics of S1 can vary in healthy individuals due to factors such as body habitus, heart position, and respiratory cycle. For example:
- Inspiration: S1 may be slightly softer during inspiration due to increased venous return and delayed right ventricular contraction.
- Expiration: S1 may be louder during expiration.
Abnormal Variations
Changes in the intensity and characteristics of S1 can indicate various cardiac conditions:
- Loud S1: A louder-than-normal S1 can be heard in conditions such as:
- Mitral stenosis: The valve leaflets are wider apart at the onset of ventricular systole, leading to a louder closure sound.
- Hyperdynamic states: Increased heart rate and force of contraction (e.g., fever, hyperthyroidism).
- Soft S1: A softer-than-normal S1 can occur in:
- Mitral regurgitation: The valve leaflets do not close properly, resulting in a softer sound.
- Heart failure: Weakened ventricular contractions produce a softer S1.
- Prolonged PR interval: The mitral and tricuspid valves may drift partially closed before ventricular contraction, leading to a softer S1.
- Variable S1: A varying intensity of S1 can be associated with:
- Atrial fibrillation: Irregular atrial contractions cause inconsistent filling of the ventricles, leading to variable S1 intensity.
- Complete heart block: The lack of synchrony between atrial and ventricular contractions causes variability in S1.
- Split S1: A split S1 can be heard when there is a significant delay between the closure of the mitral and tricuspid valves, such as in:
- Right bundle branch block (RBBB): Delayed right ventricular contraction causes the tricuspid valve to close later than the mitral valve.
- Premature ventricular contractions (PVCs): Ectopic beats can cause asynchronous valve closure.
Auscultation Techniques
Optimal Sites for Listening
To accurately assess the first heart sound, it’s essential to auscultate at specific sites on the chest wall:
- Mitral Area: Fifth intercostal space at the midclavicular line, where the mitral component (M1) is best heard.
- Tricuspid Area: Fourth or fifth intercostal space at the left sternal border, where the tricuspid component (T1) is best heard.
Techniques to Enhance Auscultation
Certain techniques can enhance the auscultation of S1:
- Patient Positioning:
- Left lateral decubitus position: Enhances the audibility of the mitral component (M1).
- Supine position: Standard position for general cardiac auscultation.
- Sitting up and leaning forward: Can enhance the audibility of S1, especially for patients with emphysema or obesity.
- Respiratory Maneuvers:
- Asking the patient to hold their breath: Can help differentiate S1 from S2.
- Deep inspiration: Can accentuate the split S1 by increasing venous return and delaying right ventricular contraction.
- Using the Bell and Diaphragm:
- Bell of the stethoscope: Better for low-frequency sounds, such as S1.
- Diaphragm of the stethoscope: Useful for high-frequency components and differentiating S1 from other sounds.
Pathological Conditions Associated with S1
Mitral Stenosis
Mitral stenosis is a condition characterized by the narrowing of the mitral valve opening, restricting blood flow from the left atrium to the left ventricle. This condition can significantly affect the characteristics of S1:
- Loud S1: The mitral valve leaflets are more widely separated at the onset of systole due to the increased left atrial pressure, resulting in a louder closure sound.
- Opening Snap: An additional sound heard shortly after S2, due to the abrupt halting of the stiff mitral valve leaflets during diastole.
Mitral Regurgitation
Mitral regurgitation occurs when the mitral valve does not close properly, allowing blood to flow backward into the left atrium during ventricular contraction. This condition affects S1 in the following ways:
- Soft S1: The mitral valve leaflets do not close completely, resulting in a softer closure sound.
- Holosystolic Murmur: A continuous murmur heard throughout systole, often obscuring S1.
Right Bundle Branch Block (RBBB)
RBBB is a condition where the right bundle branch of the heart’s conduction system is blocked, delaying right ventricular contraction. This delay affects the timing of the tricuspid valve closure, leading to:
- Split S1: A noticeable delay between the closure of the mitral (M1) and tricuspid (T1) valves, resulting in a split S1 sound.
Heart Failure
Heart failure, particularly left ventricular dysfunction, can affect the intensity of S1:
- Soft S1: Weakened ventricular contractions produce a softer S1 due to reduced force in closing the mitral and tricuspid valves.
- Variable S1: Variability in S1 intensity due to irregular ventricular contractions.
Diagnostic Tools and Techniques
Electrocardiography (ECG)
An electrocardiogram (ECG) is a vital tool in diagnosing conditions that affect S1. The QRS complex on an ECG represents ventriculardepolarization and is synchronous with the first heart sound (S1). By analyzing the timing and morphology of the QRS complex, clinicians can gain insights into conditions such as bundle branch blocks, which affect the timing of valve closures and consequently the characteristics of S1.
Echocardiography
Echocardiography is an essential imaging modality that provides detailed information about the structure and function of the heart valves and chambers. Through techniques such as Doppler echocardiography, clinicians can visualize blood flow patterns, detect valve abnormalities, and measure the severity of conditions like mitral stenosis or regurgitation. This helps in correlating the auscultatory findings with anatomical and functional abnormalities.
Phonocardiography
Phonocardiography involves the recording of heart sounds using specialized microphones and electronic equipment. This technique allows for the visual representation of heart sounds, facilitating the identification and analysis of abnormal heart sounds, including variations in S1. Phonocardiograms can be particularly useful in research settings and for teaching purposes, providing an objective method to study heart sounds.
Clinical Case Studies
Case Study 1: Mitral Stenosis
A 45-year-old female presents with progressive shortness of breath and fatigue. On physical examination, a loud S1 and an opening snap are noted, followed by a diastolic rumble best heard at the apex in the left lateral decubitus position. Echocardiography confirms the diagnosis of mitral stenosis with a markedly narrowed mitral valve orifice.
- Interpretation: The loud S1 is due to the increased separation of the mitral valve leaflets at the onset of systole, resulting in a more forceful closure. The opening snap is a high-pitched sound caused by the abrupt halting of the stiff mitral valve leaflets during diastole.
Case Study 2: Mitral Regurgitation
A 60-year-old male with a history of hypertension presents with complaints of palpitations and occasional chest pain. Auscultation reveals a soft S1 and a holosystolic murmur radiating to the axilla. Echocardiography shows a dilated left atrium and left ventricle with moderate mitral regurgitation.
- Interpretation: The soft S1 is due to the incomplete closure of the mitral valve, allowing blood to flow back into the left atrium during systole. The holosystolic murmur is characteristic of mitral regurgitation and masks the first heart sound.
Conclusion
The first heart sound (S1) is a critical auditory marker in cardiac auscultation, providing valuable information about the mechanical events occurring at the onset of ventricular systole. Understanding the factors that influence the intensity and characteristics of S1 is essential for accurate diagnosis and management of various cardiac conditions. Through auscultation, combined with diagnostic tools such as ECG, echocardiography, and phonocardiography, clinicians can effectively evaluate and monitor heart health, ensuring timely and appropriate interventions.
By appreciating the nuances of S1 and its variations, healthcare providers can enhance their diagnostic acumen and improve patient outcomes. Regular practice and continued education in auscultation techniques remain fundamental in mastering the art of cardiac assessment.
Sure, here is the information presented in a linked format:
- Leng, S; Tan, R; Chai, R; Wang, C (2015). “The electronic stethoscope”. BioMedical Engineering OnLine. 14 (1): 66. doi:10.1186/s12938-015-0056-y. PMC 4496820. PMID 26159433. Retrieved 30 June 2021.
- “Techniques – Heart Sounds & Murmurs Exam – Physical Diagnosis Skills”. University of Washington School of Medicine.
- “Aortic Regurgitation”. The Lecturio Medical Concept Library. October 2020. Retrieved 30 June 2021.
- “thrill”. Archived 2011-05-27 at the Wayback Machine Medline Plus Medical Dictionary.
- Bernstein, Lenny (2016-01-02), “Heart doctors are listening for clues to the future of their stethoscopes”. Washington Post, archived from the original on 2016-01-09.
- Mallinson, T (2017). “A survey into paramedic accuracy in identifying the correct anatomic locations for cardiac auscultation”. British Paramedic Journal. 2 (2): 13–17. doi:10.29045/14784726.2017.2.2.13.
Read-




