The heart is a vital organ that functions ceaselessly to pump blood throughout the body, and its sounds can reveal a lot about cardiovascular health. The heart sounds, including the first heart sound (S1) and the second heart sound (S2), are integral to clinical diagnosis. In this blog post, we will delve into the second heart sound (S2), its physiology, clinical significance, and the conditions that affect it.
Anatomy and Physiology of Heart Sounds
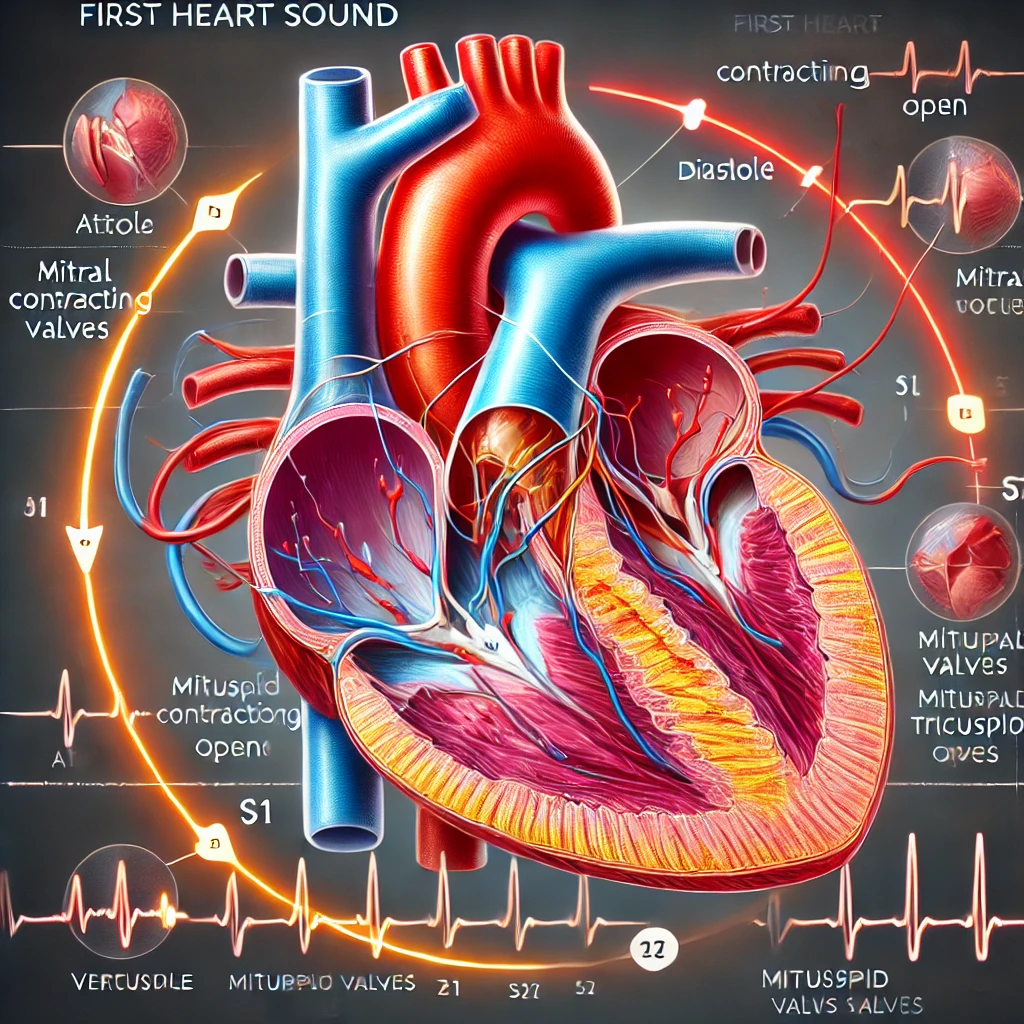
The First Heart Sound (S1)
The first heart sound, often described as the “lub” in the “lub-dub” sequence, is primarily produced by the closing of the atrioventricular (AV) valves, which include the mitral and tricuspid valves. This sound marks the onset of ventricular systole, the phase of the cardiac cycle when the ventricles contract to eject blood into the aorta and pulmonary artery. The S1 sound can be best heard at the apex of the heart, typically located in the fifth intercostal space at the midclavicular line.
The intensity of S1 can be influenced by several factors, including the position of the AV valves at the onset of systole, the force of ventricular contraction, and the velocity of blood flow through the valves. Variations in S1 can provide important diagnostic clues. For example, a louder S1 may indicate conditions such as mitral stenosis, while a softer S1 could suggest mitral regurgitation or left ventricular dysfunction.
The mitral and tricuspid valves function as gateways between the atria and ventricles. During diastole, these valves open to allow blood to flow from the atria into the ventricles. At the onset of systole, the ventricles contract, causing a rapid increase in pressure that forces the AV valves to snap shut, producing the S1 sound. The closure of these valves prevents the backflow of blood into the atria, ensuring unidirectional blood flow through the heart.
The timing and quality of S1 can be affected by various physiological and pathological conditions. For instance, the PR interval on an electrocardiogram (ECG) reflects the time between atrial and ventricular depolarization. A prolonged PR interval can delay the closure of the AV valves, leading to a softer S1. Conversely, a shortened PR interval can result in a louder S1 due to the rapid onset of ventricular contraction.
In addition to the AV valves, the structure and function of the myocardium play a role in the generation of S1. The myocardium is composed of specialized cardiac muscle cells that contract in a coordinated manner to pump blood. Factors that affect myocardial contractility, such as electrolyte imbalances, ischemia, or hypertrophy, can influence the intensity and quality of S1.
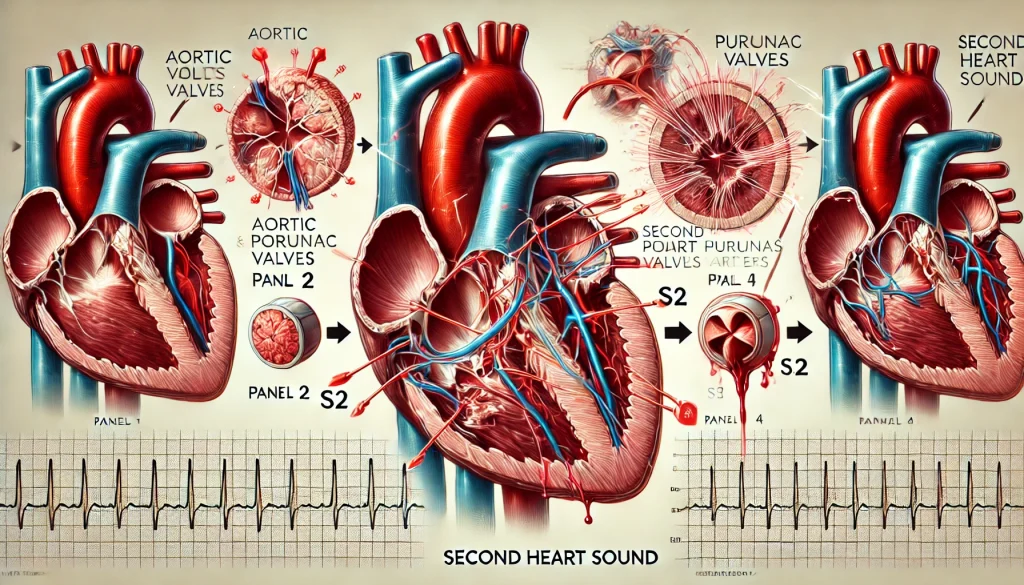
The Second Heart Sound (S2)
The second heart sound, commonly referred to as the “dub” in the “lub-dub” sequence, is generated by the closing of the semilunar valves—the aortic and pulmonary valves. This sound marks the end of ventricular systole and the beginning of ventricular diastole, when the ventricles relax and fill with blood. S2 is shorter and higher-pitched compared to S1 and is best heard at the base of the heart, particularly at the second intercostal space along the left and right sternal borders.
The second heart sound is produced by the closure of the semilunar valves, which prevent the backflow of blood from the aorta and pulmonary artery into the ventricles. During systole, the ventricles contract, forcing blood through the aortic and pulmonary valves into the systemic and pulmonary circulations, respectively. As ventricular contraction ends, the pressure in the aorta and pulmonary artery exceeds that in the ventricles, causing the semilunar valves to close. The sudden deceleration of blood flow and the resultant vibration of the valve leaflets produce the S2 sound.
S2 consists of two components:
- Aortic Component (A2): The sound produced by the closure of the aortic valve.
- Pulmonary Component (P2): The sound produced by the closure of the pulmonary valve.
Under normal physiological conditions, the aortic valve closes slightly before the pulmonary valve due to the higher pressure in the systemic circulation compared to the pulmonary circulation. This slight delay results in the splitting of S2.
The timing and quality of S2 can provide valuable information about cardiac function and hemodynamics. The interval between A2 and P2 can be influenced by factors such as intrathoracic pressure, ventricular compliance, and the duration of ventricular systole. For instance, during inspiration, the negative intrathoracic pressure increases venous return to the right side of the heart, prolonging right ventricular systole and delaying P2. This physiological splitting of S2 is a normal finding in healthy individuals.
The quality of S2 can also provide diagnostic clues. A loud and sharp S2 may indicate increased pressure in the aorta or pulmonary artery, as seen in conditions such as systemic hypertension or pulmonary hypertension. Conversely, a soft or muffled S2 may suggest valve dysfunction or reduced cardiac output. The presence of additional heart sounds, such as a third heart sound (S3) or fourth heart sound (S4), can further complicate the interpretation of S2 and may indicate underlying cardiac pathology.
Components of the Second Heart Sound
Aortic Component (A2)
The aortic component of the second heart sound (A2) is typically louder and occurs earlier than the pulmonary component (P2). This is due to the higher pressure in the aorta, which causes the aortic valve to close with greater force and speed. A2 is best heard at the right upper sternal border, in the second intercostal space. The intensity and timing of A2 can provide important diagnostic information. For example, an abnormally loud A2 may indicate systemic hypertension, while a diminished A2 could suggest aortic stenosis or regurgitation.
The closure of the aortic valve is a critical event in the cardiac cycle. During systole, the left ventricle contracts and ejects blood into the aorta, generating a high-pressure gradient across the aortic valve. As ventricular contraction ends and the pressure in the aorta exceeds that in the left ventricle, the aortic valve closes to prevent the backflow of blood. The forceful closure of the aortic valve and the resultant vibration of the valve leaflets produce the A2 component of the second heart sound.
The timing of A2 relative to the pulmonary component (P2) can provide insights into ventricular function and hemodynamics. In healthy individuals, A2 occurs slightly before P2 due to the higher pressure in the aorta compared to the pulmonary artery. This normal sequence of events results in the physiological splitting of S2 during inspiration. However, pathological conditions that alter ventricular pressure or volume can affect the timing of A2 and P2, leading to abnormal splitting of S2.
The intensity of A2 can also provide diagnostic clues about the condition of the aortic valve and the systemic circulation. For instance, a loud A2 may indicate elevated aortic pressure, as seen in systemic hypertension or hyperthyroidism. Conversely, a soft or diminished A2 may suggest aortic stenosis, where the calcified and narrowed aortic valve fails to close properly. Aortic regurgitation, where the aortic valve does not close completely, can also result in a decreased intensity of A2.
Pulmonary Component (P2)
The pulmonary component of the second heart sound (P2) is softer and follows A2. It is best heard at the left upper sternal border, in the second intercostal space. The intensity of P2 can be affected by various factors, including pulmonary artery pressure and the condition of the pulmonary valve. For instance, a loud P2 is often associated with pulmonary hypertension, while a soft P2 may indicate pulmonary stenosis or other pulmonary disorders.
The closure of the pulmonary valve is a key event in the cardiac cycle, marking the end of right ventricular systole. During systole, the right ventricle contracts and ejects blood into the pulmonary artery, generating a pressure gradient across the pulmonary valve. As ventricular contraction ends and the pressure in the pulmonary artery exceeds that in the right ventricle, the pulmonary valve closes to prevent the backflow of blood. The closure of the pulmonary valve and the resultant vibration of the valve leaflets produce the P2 component of the second heart sound.
The timing of P2 relative to A2 can provide valuable information about right ventricular function and pulmonary hemodynamics. In healthy individuals, P2 occurs slightly after A2 due to the lower pressure in the pulmonary artery compared to the aorta. This normal sequence of events results in the physiological splitting of S2 during inspiration. However, pathological conditions that alter right ventricular pressure or volume can affect the timing of P2, leading to abnormal splitting of S2.
The intensity of P2 can also provide diagnostic clues about the condition of the pulmonary valve and the pulmonary circulation. For example, a loud P2 may indicate elevated pulmonary artery pressure, as seen in pulmonary hypertension. This condition can result from various causes, including chronic lung disease, left heart disease, or thromboembolic disease. Conversely, a soft or diminished P2 may suggest pulmonary stenosis, where the narrowed pulmonary valve fails to close properly. Severe COPD, which reduces pulmonary circulation pressure, can also result in a decreased intensity of P2.
Splitting of S2
Physiological Splitting
In a healthy heart, the splitting of S2 varies with the respiratory cycle. During inspiration, the negative intrathoracic pressure increases venous return to the right side of the heart, leading to a prolonged right ventricular systole and a delayed closure of the pulmonary valve (P2). This results in a wider splitting of S2. During expiration, the venous return decreases, and the splitting narrows as P2 occurs earlier.
Physiological splitting of S2 is a normal finding in healthy individuals and is influenced by the mechanics of respiration and intrathoracic pressure. During inspiration, the negative intrathoracic pressure enhances venous return to the right atrium, increasing right ventricular preload and stroke volume. The increased volume of blood in the right ventricle prolongs right ventricular systole and delays the closure of the pulmonary valve, resulting in a wider splitting of S2.
The splitting of S2 can be best appreciated at the left upper sternal border, where the pulmonary component (P2) is more prominent. The degree of splitting can vary among individuals and may be influenced by factors such as age, body habitus, and respiratory effort. In some individuals, the splitting of S2 may be barely perceptible, while in others, it may be more pronounced.
Wide Splitting
Wide splitting of S2, which persists throughout the respiratory cycle, can be indicative of conditions that delay right ventricular systole. Examples include right bundle branch block (RBBB) and pulmonary stenosis. In RBBB, the electrical conduction to the right ventricle is delayed, causing prolonged right ventricular contraction and delayed P2. In pulmonary stenosis, the obstruction of blood flow through the pulmonary valve prolongs right ventricular systole and delays P2.
Right bundle branch block (RBBB) is a conduction abnormality that results in delayed depolarization and contraction of the right ventricle. This delay prolongs right ventricular systole and causes persistent wide splitting of S2, regardless of the respiratory cycle. An electrocardiogram (ECG) is typically required to confirm the diagnosis of RBBB, revealing characteristic findings such as an rsR’ pattern in lead V1 and a wide QRS complex.
Pulmonary stenosis is a condition characterized by the narrowing of the pulmonary valve, which obstructs blood flow from the right ventricle into the pulmonary artery. The increased resistance to blood flow prolongs right ventricular systole and delays the closure of the pulmonary valve, resulting in wide splitting of S2. Auscultation may reveal a systolic ejection murmur at the left upper sternal border, along with a prominent P2 component.
Fixed Splitting
Fixed splitting of S2, where the split remains constant regardless of the respiratory cycle, is a hallmark of atrial septal defect (ASD). In ASD, the left-to-right shunt of blood increases right ventricular volume and delays P2 consistently throughout the respiratory cycle.
Atrial septal defect (ASD) is a congenital heart defect characterized by an abnormal opening in the atrial septum, allowing blood to flow between the left and right atria. This left-to-right shunt increases right atrial and right ventricular volume, leading to prolonged right ventricular systole and delayed closure of the pulmonary valve. The result is fixed splitting of S2, where the split remains constant during both inspiration and expiration.
ASD can be associated with other clinical findings, such as a systolic ejection murmur at the left upper sternal border and a diastolic rumble at the lower left sternal border. Echocardiography is the diagnostic modality of choice for confirming the presence and size of the atrial septal defect, as well as assessing its hemodynamic impact.
Paradoxical Splitting
Paradoxical or reversed splitting of S2 occurs when the aortic valve closure (A2) is delayed, causing P2 to occur before A2. This is seen in conditions that delay left ventricular systole, such as left bundle branch block (LBBB) and aortic stenosis. In LBBB, the electrical conduction to the left ventricle is delayed, resulting in prolonged left ventricular contraction and delayed A2. In aortic stenosis, the narrowing of the aortic valve prolongs left ventricular systole and delays A2.
Left bundle branch block (LBBB) is a conduction abnormality that results in delayed depolarization and contraction of the left ventricle. This delay prolongs left ventricular systole and causes paradoxical splitting of S2, where the aortic component (A2) is delayed and follows the pulmonary component (P2). An ECG is necessary to confirm the diagnosis of LBBB, showing broad, notched R waves in leads I, aVL, V5, and V6.
Aortic stenosis is a condition characterized by the narrowing of the aortic valve, which obstructs blood flow from the left ventricle into the aorta. The increased resistance to blood flow prolongs left ventricular systole and delays the closure of the aortic valve, resulting in paradoxical splitting of S2. Auscultation typically reveals a harsh systolic murmur at the right upper sternal border, radiating to the neck. Echocardiography is the gold standard for assessing the severity of aortic stenosis and planning appropriate interventions.
Clinical Significance of the Second Heart Sound
Intensity of S2
The intensity of S2 can provide valuable diagnostic information about the pressure and condition of the aortic and pulmonary circulations.
- Increased A2: An abnormally loud A2 may indicate elevated aortic pressure, as seen in systemic hypertension. It can also occur in conditions that increase the force of aortic valve closure, such as hyperthyroidism or coarctation of the aorta.
- Decreased A2: A soft or diminished A2 can suggest aortic stenosis, where the calcified and narrowed aortic valve fails to close properly. Aortic regurgitation, where the aortic valve does not close completely, can also result in a decreased A2.
- Increased P2: A loud P2 is commonly associated with pulmonary hypertension, where elevated pressure in the pulmonary artery causes a forceful closure of the pulmonary valve.
- Decreased P2: A soft P2 may indicate pulmonary stenosis, where the pulmonary valve is narrowed, or severe COPD, where the pulmonary circulation pressure is reduced.
The intensity of the second heart sound (S2) can provide valuable insights into the pressure and condition of the aortic and pulmonary circulations. Variations in the intensity of S2 components (A2 and P2) can indicate specific cardiac or pulmonary conditions.
Increased Intensity of A2
An abnormally loud aortic component (A2) may indicate elevated aortic pressure. This can be seen in conditions such as systemic hypertension, where the increased systemic vascular resistance results in higher aortic pressure and a forceful closure of the aortic valve. Other conditions that can increase the intensity of A2 include hyperthyroidism, which increases metabolic demand and cardiac output, and coarctation of the aorta, a congenital narrowing of the aorta that leads to elevated pressure proximal to the obstruction.
In systemic hypertension, the increased pressure in the aorta forces the aortic valve to close with greater force, resulting in a loud A2. The heightened intensity of A2 can be appreciated during auscultation at the right upper sternal border. In addition to the loud A2, patients with systemic hypertension may present with other signs and symptoms, such as elevated blood pressure, left ventricular hypertrophy, and hypertensive retinopathy.
Decreased Intensity of A2
A soft or diminished A2 can suggest aortic stenosis, where the calcified and narrowed aortic valve fails to close properly. In aortic stenosis, the thickened and immobile valve leaflets reduce the intensity of the sound produced during closure. Aortic regurgitation, where the aortic valve does not close completely, can also result in a decreased A2. In this condition, the backflow of blood into the left ventricle during diastole reduces the force of valve closure, leading to a softer A2.
In patients with aortic stenosis, auscultation may reveal a soft or diminished A2, along with a harsh, crescendo-decrescendo systolic murmur at the right upper sternal border. The murmur typically radiates to the carotid arteries. Echocardiography is essential for confirming the diagnosis and assessing the severity of the stenosis.
Increased Intensity of P2
A loud pulmonary component (P2) is commonly associated with pulmonary hypertension, where elevated pressure in the pulmonary artery causes a forceful closure of the pulmonary valve. Pulmonary hypertension can result from various underlying conditions, including chronic lung disease, left heart disease, and thromboembolic disease. The increased resistance in the pulmonary circulation leads to elevated right ventricular pressure and a forceful closure of the pulmonary valve, resulting in a loud P2.
In patients with pulmonary hypertension, auscultation may reveal a loud P2, best heard at the left upper sternal border. Additional findings may include a systolic ejection click and signs of right ventricular hypertrophy, such as a right ventricular heave or palpable impulse. Further evaluation with echocardiography and right heart catheterization is necessary to confirm the diagnosis and assess the severity of pulmonary hypertension.
Decreased Intensity of P2
A soft or diminished P2 may indicate pulmonary stenosis, where the pulmonary valve is narrowed and fails to close properly. In pulmonary stenosis, the thickened and immobile valve leaflets reduce the intensity of the sound produced during closure. Severe chronic obstructive pulmonary disease (COPD) can also result in a decreased intensity of P2, as the reduced pulmonary circulation pressure decreases the force of valve closure.
In patients with pulmonary stenosis, auscultation may reveal a soft or diminished P2, along with a systolic ejection murmur at the left upper sternal border. The murmur may radiate to the back or neck. Echocardiography is essential for confirming the diagnosis and assessing the severity of the stenosis.
Pathological Conditions Affecting S2
Aortic Stenosis
Aortic stenosis is a condition characterized by the narrowing of the aortic valve, leading to obstructed blood flow from the left ventricle into the aorta. This obstruction results in a decreased intensity of A2 and can cause paradoxical splitting of S2. Auscultation typically reveals a harsh systolic murmur, best heard at the right upper sternal border, and radiating to the carotid arteries.
Aortic stenosis is most commonly caused by age-related degenerative changes, leading to calcification and thickening of the aortic valve leaflets. Other causes include congenital bicuspid aortic valve and rheumatic heart disease. The narrowed valve obstructs blood flow, increasing the pressure gradient across the valve and resulting in left ventricular hypertrophy.
Patients with aortic stenosis may present with symptoms such as chest pain, syncope, and dyspnea on exertion. The decreased intensity of A2 is due to the reduced mobility of the calcified valve leaflets, which fail to close properly. Paradoxical splitting of S2 occurs because the prolonged left ventricular systole delays the closure of the aortic valve, causing A2 to follow P2.
Diagnosis of aortic stenosis is confirmed through echocardiography, which provides detailed information about the valve anatomy, pressure gradient, and left ventricular function. Management options include medical therapy for symptom relief and surgical intervention, such as aortic valve replacement, for severe cases.
Pulmonary Hypertension
Pulmonary hypertension is defined as elevated pressure in the pulmonary arteries. This condition can result in a loud P2 due to the increased force required to close the pulmonary valve. Auscultation may reveal an accentuated P2 and a possible systolic ejection click. Pulmonary hypertension can be primary or secondary to various conditions, such as chronic lung disease, left heart disease, or thromboembolic disease.
Pulmonary hypertension can be classified into five groups based on the underlying cause: pulmonary arterial hypertension, pulmonary hypertension due to left heart disease, pulmonary hypertension due to lung diseases or hypoxia, chronic thromboembolic pulmonary hypertension, and pulmonary hypertension with unclear multifactorial mechanisms.
The increased pressure in the pulmonary arteries leads to right ventricular hypertrophy and eventual right heart failure if left untreated. The loud P2 is a result of the forceful closure of the pulmonary valve due to the elevated pulmonary artery pressure.
Diagnosis of pulmonary hypertension involves a combination of clinical assessment, imaging studies, and hemodynamic measurements. Echocardiography can estimate pulmonary artery pressure and assess right ventricular function. Right heart catheterization is the gold standard for confirming the diagnosis and measuring pulmonary artery pressure.
Management of pulmonary hypertension depends on the underlying cause and may include medications such as vasodilators, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors. In some cases, advanced therapies such as lung transplantation may be considered.
Atrial Septal Defect (ASD)
An atrial septal defect is a congenital heart defect characterized by an abnormal opening in the atrial septum, allowing blood to flow between the left and right atria. This results in increased right ventricular volume and delayed closure of the pulmonary valve, leading to a fixed splitting of S2. Auscultation may reveal a systolic ejection murmur at the left upper sternal border and a diastolic rumble at the lower left sternal border.
ASD is one of the most common congenital heart defects and can vary in size and location within the atrial septum. The left-to-right shunt increases right atrial and right ventricular volume, leading to prolonged right ventricular systole and delayed closure of the pulmonary valve. The fixed splitting of S2 is a characteristic finding in ASD, as the split remains constant during both inspiration and expiration.
Patients with ASD may be asymptomatic or present with symptoms such as palpitations, fatigue, and exercise intolerance. Large defects can lead to complications such as atrial arrhythmias, pulmonary hypertension, and right heart failure.
Diagnosis of ASD is confirmed through echocardiography, which provides detailed information about the size and location of the defect, as well as the hemodynamic impact. Management options include medical therapy for symptom relief and percutaneous or surgical closure of the defect.
Right Bundle Branch Block (RBBB)
Right bundle branch block is a conduction abnormality where the right bundle branch of the heart’s electrical conduction system is blocked. This causes delayed right ventricular depolarization and prolonged right ventricular systole, resulting in wide splitting of S2. An ECG is typically required to confirm the diagnosis, revealing characteristic findings such as an rsR’ pattern in lead V1.
RBBB can be caused by various conditions, including congenital heart disease, myocardial infarction, and degenerative changes in the conduction system. The delayed depolarization and contraction of the right ventricle result in prolonged right ventricular systole and delayed closure of the pulmonary valve, leading to wide splitting of S2.
Patients with RBBB may be asymptomatic or present with symptoms such as palpitations, syncope, or dyspnea. The wide splitting of S2 can be appreciated during auscultation, and the diagnosis is confirmed through ECG, which shows characteristic findings of RBBB.
Management of RBBB depends on the underlying cause and the presence of symptoms. In asymptomatic patients, no specific treatment may be required. In patients with underlying cardiac conditions or symptoms, further evaluation and management are necessary.
Left Bundle Branch Block (LBBB)
Left bundle branch block is a conduction abnormality where the left bundle branch is blocked, causing delayed left ventricular depolarization. This condition can lead to paradoxical splitting of S2, with delayed closure of the aortic valve. An ECG is necessary for diagnosis, showing broad, notched R waves in leads I, aVL, V5, and V6.
LBBB can be caused by various conditions, including myocardial infarction, cardiomyopathy, and degenerative changes in the conduction system. The delayed depolarization and contraction of the left ventricle result in prolonged left ventricular systole and delayed closure of the aortic valve, causing paradoxical splitting of S2.
Patients with LBBB may be asymptomatic or present with symptoms such as palpitations, syncope, or heart failure. The paradoxical splitting of S2 can be appreciated during auscultation, and the diagnosis is confirmed through ECG, which shows characteristic findings of LBBB.
Management of LBBB depends on the underlying cause and the presence of symptoms. In asymptomatic patients, no specific treatment may be required. In patients with underlying cardiac conditions or symptoms, further evaluation and management are necessary.
Aortic Regurgitation
Aortic regurgitation is a condition where the aortic valve fails to close properly, allowing blood to flow back into the left ventricle from the aorta during diastole. This condition results in a decreased intensity of A2 and a high-pitched, blowing diastolic murmur heard best at the left sternal border. Chronic aortic regurgitation can lead to left ventricular dilation and heart failure if left untreated.
Aortic regurgitation can be caused by various conditions, including aortic valve degeneration, endocarditis, and aortic root dilation. The backflow of blood into the left ventricle during diastole increases left ventricular volume and pressure, leading to left ventricular hypertrophy and dilation.
Patients with aortic regurgitation may present with symptoms such as palpitations, dyspnea, and chest pain. The decreased intensity of A2 is due to the reduced force of valve closure, as the aortic valve fails to close completely. The high-pitched, blowing diastolic murmur is best heard at the left sternal border and may radiate to the apex.
Diagnosis of aortic regurgitation is confirmed through echocardiography, which provides detailed information about the valve anatomy, regurgitant volume, and left ventricular function. Management options include medical therapy for symptom relief and surgical intervention, such as aortic valve replacement, for severe cases.
Diagnostic Techniques for Evaluating S2
Auscultation
Auscultation with a stethoscope remains the primary method for assessing heart sounds, including S2. Clinicians listen for the intensity, timing, and splitting of S2 to gather diagnostic clues. Proper technique and a quiet environment are essential for accurate auscultation. Listening at various sites on the chest, including the aortic, pulmonic, tricuspid, and mitral areas, can help identify the best locations for hearing A2 and P2.
Auscultation is a fundamental skill in clinical practice and provides valuable information about cardiac function. During auscultation, clinicians use a stethoscope to listen to heart sounds at specific locations on the chest, known as auscultatory areas. These areas correspond to the locations where heart sounds are best heard based on the anatomy of the heart and great vessels.
- Aortic Area: Located at the right upper sternal border in the second intercostal space. This area is best for hearing the aortic component (A2) of S2.
- Pulmonic Area: Located at the left upper sternal border in the second intercostal space. This area is best for hearing the pulmonary component (P2) of S2.
- Tricuspid Area: Located at the lower left sternal border in the fourth or fifth intercostal space. This area is best for hearing tricuspid valve sounds.
- Mitral Area: Located at the apex of the heart in the fifth intercostal space at the midclavicular line. This area is best for hearing mitral valve sounds.
The intensity, timing, and splitting of S2 can provide important diagnostic information. For example, a loud A2 may indicate systemic hypertension, while a soft P2 may suggest pulmonary stenosis. The presence of physiological splitting of S2 during inspiration is a normal finding, while wide or fixed splitting can indicate underlying cardiac conditions.
Phonocardiography
Phonocardiography involves recording heart sounds using a microphone and visualizing them on a phonocardiogram. This technique provides a graphical representation of heart sounds, allowing for detailed analysis of the frequency, amplitude, and duration of S2. Phonocardiography can be particularly useful in research settings and in cases where auscultation findings are unclear.
Phonocardiography provides an objective method for analyzing heart sounds and can complement clinical auscultation. The phonocardiogram displays heart sounds as waveforms, with peaks corresponding to the intensity and frequency of each sound. This visualization allows clinicians to analyze the timing, duration, and splitting of S2 more accurately.
The use of phonocardiography can aid in the diagnosis of various cardiac conditions. For example, the presence of wide splitting of S2 can be quantified and analyzed, providing additional information about the underlying cause. Phonocardiography can also be used to monitor changes in heart sounds over time, helping to assess the effectiveness of treatments and interventions.
Echocardiography
Echocardiography uses ultrasound waves to create images of the heart and its structures. This non-invasive technique provides detailed information about heart valves, chamber sizes, and blood flow. Doppler echocardiography can assess the velocity and direction of blood flow, aiding in the diagnosis of conditions affecting S2, such as aortic or pulmonary valve disorders. Echocardiography is considered the gold standard for evaluating structural heart diseases.
Echocardiography is a versatile diagnostic tool that provides comprehensive information about cardiac anatomy and function. The use of ultrasound allows for real-time visualization of the heart, enabling the assessment of valve morphology, chamber sizes, and ventricular function.
- Two-Dimensional Echocardiography: Provides cross-sectional images of the heart, allowing for the evaluation of structural abnormalities, such as valve stenosis or regurgitation.
- Doppler Echocardiography: Measures the velocity and direction of blood flow, providing information about pressure gradients across valves and the presence of abnormal flow patterns.
- Color Doppler Imaging: Visualizes blood flow in color, helping to identify areas of turbulent or abnormal flow, such as regurgitant jets.
Echocardiography is essential for diagnosing conditions that affect the second heart sound. For example, aortic stenosis can be confirmed by visualizing the calcified and narrowed aortic valve and measuring the pressure gradient across the valve. Pulmonary hypertension can be assessed by estimating pulmonary artery pressure and evaluating right ventricular function.
Electrocardiography (ECG)
Electrocardiography records the electrical activity of the heart and helps identify conduction abnormalities that affect the timing of S2. An ECG can reveal characteristic patterns associated with conditions like right or left bundle branch blocks, which influence the splitting of S2. Combining ECG findings with auscultation and echocardiography can provide a comprehensive assessment of cardiac function.
ECG is a widely used diagnostic tool that provides valuable information about the heart’s electrical activity. The ECG tracing consists of waveforms that represent different phases of the cardiac cycle, including atrial and ventricular depolarization and repolarization.
- P Wave: Represents atrial depolarization.
- QRS Complex: Represents ventricular depolarization.
- T Wave: Represents ventricular repolarization.
Conduction abnormalities, such as right or left bundle branch blocks, can affect the timing of ventricular depolarization and contraction, leading to abnormal splitting of S2. In right bundle branch block (RBBB), the delayed depolarization of the right ventricle results in wide splitting of S2. In left bundle branch block (LBBB), the delayed depolarization of the left ventricle results in paradoxical splitting of S2.
The combination of ECG findings with clinical auscultation and echocardiography provides a comprehensive assessment of cardiac function. For example, an ECG showing an rsR’ pattern in lead V1 and a wide QRS complex can confirm the diagnosis of RBBB, while echocardiography can further evaluate the impact of the conduction abnormality on right ventricular function.
Clinical Cases Involving S2
Case 1: Aortic Stenosis
A 70-year-old male presents with chest pain and shortness of breath on exertion. On auscultation, a soft A2 and paradoxical splitting of S2 are noted. The patient’s history includes episodes of syncope and a crescendo-decrescendo systolic murmur radiating to the neck. Echocardiography reveals a heavily calcified and stenotic aortic valve with a reduced aortic valve area. The diagnosis of aortic stenosis is confirmed, and the patient is referred for aortic valve replacement surgery. Postoperative follow-up shows significant improvement in symptoms and normalization of S2 splitting.
Aortic stenosis is a common valvular heart disease, particularly in older adults, and is characterized by the narrowing of the aortic valve. The most common cause of aortic stenosis is age-related degenerative changes, leading to calcification and thickening of the valve leaflets. Other causes include congenital bicuspid aortic valve and rheumatic heart disease.
The decreased intensity of A2 in aortic stenosis is due to the reduced mobility of the calcified valve leaflets, which fail to close properly. The paradoxical splitting of S2 occurs because the prolonged left ventricular systole delays the closure of the aortic valve, causing A2 to follow P2. Auscultation typically reveals a harsh, crescendo-decrescendo systolic murmur at the right upper sternal border, radiating to the neck. The murmur is caused by the turbulent flow of blood through the narrowed valve.
Echocardiography is essential for diagnosing aortic stenosis and assessing its severity. The echocardiogram provides detailed information about the valve anatomy, pressure gradient across the valve, and left ventricular function. In this case, the echocardiogram reveals a heavily calcified and stenotic aortic valve with a reduced aortic valve area, confirming the diagnosis.
Management of aortic stenosis depends on the severity of the condition and the presence of symptoms. In patients with severe aortic stenosis and symptoms such as chest pain, syncope, or heart failure, surgical intervention is necessary. Aortic valve replacement is the definitive treatment for severe aortic stenosis and can significantly improve symptoms and survival. Postoperative follow-up is essential to monitor valve function and assess the patient’s clinical status.
Case 2: Pulmonary Hypertension
A 45-year-old female with a history of systemic sclerosis presents with fatigue and dyspnea. On auscultation, a loud P2 and wide splitting of S2 are observed. Further evaluation with echocardiography and right heart catheterization confirms the diagnosis of pulmonary hypertension, revealing elevated pulmonary artery pressures. The patient is started on targeted therapy for pulmonary hypertension, including endothelin receptor antagonists and phosphodiesterase-5 inhibitors. Regular follow-up and monitoring show stabilization of pulmonary pressures and improvement in exercise tolerance.
Pulmonary hypertension is a condition characterized by elevated pressure in the pulmonary arteries, leading to increased right ventricular workload and eventual right heart failure if left untreated. Pulmonary hypertension can be primary (idiopathic) or secondary to various conditions, such as chronic lung disease, left heart disease, and thromboembolic disease.
The loud P2 in pulmonary hypertension is a result of the forceful closure of the pulmonary valve due to the elevated pulmonary artery pressure. The wide splitting of S2 is caused by the prolonged right ventricular systole, which delays the closure of the pulmonary valve. Auscultation reveals an accentuated P2 and a possible systolic ejection click, indicating elevated pulmonary pressures.
Echocardiography is a non-invasive tool that can estimate pulmonary artery pressure and assess right ventricular function. In this case, echocardiography reveals elevated pulmonary artery pressures and signs of right ventricular hypertrophy. Right heart catheterization is the gold standard for confirming the diagnosis and measuring pulmonary artery pressure.
Management of pulmonary hypertension involves a combination of targeted therapies and supportive care. Endothelin receptor antagonists and phosphodiesterase-5 inhibitors are commonly used to reduce pulmonary vascular resistance and improve symptoms. Regular follow-up and monitoring are essential to assess treatment response and adjust therapy as needed. In severe cases, advanced therapies such as lung transplantation may be considered.
Case 3: Atrial Septal Defect
A 25-year-old female presents with palpitations and exercise intolerance. On auscultation, a fixed splitting of S2 is heard, along with a systolic ejection murmur at the left upper sternal border. Echocardiography reveals a secundum atrial septal defect with significant left-to-right shunting. The patient undergoes percutaneous closure of the defect using a transcatheter device. Follow-up echocardiography confirms successful closure of the defect, and the patient’s symptoms improve significantly.
Atrial septal defect (ASD) is a congenital heart defect characterized by an abnormal opening in the atrial septum, allowing blood to flow between the left and right atria. This left-to-right shunt increases right atrial and right ventricular volume, leading to prolonged right ventricular systole and delayed closure of the pulmonary valve. The fixed splitting of S2 is a characteristic finding in ASD, as the split remains constant during both inspiration and expiration.
ASD can vary in size and location within the atrial septum, with the secundum type being the most common. Patients with ASD may be asymptomatic or present with symptoms such as palpitations, fatigue, and exercise intolerance. Large defects can lead to complications such as atrial arrhythmias, pulmonary hypertension, and right heart failure.
Diagnosis of ASD is confirmed through echocardiography, which provides detailed information about the size and location of the defect, as well as the hemodynamic impact. In this case, echocardiography reveals a secundum atrial septal defect with significant left-to-right shunting.
Management of ASD depends on the size of the defect and the presence of symptoms. Small defects may close spontaneously and may not require intervention. In patients with significant shunting and symptoms, percutaneous or surgical closure of the defect is recommended. In this case, the patient undergoes percutaneous closure of the defect using a transcatheter device. Follow-up echocardiography confirms successful closure of the defect, and the patient’s symptoms improve significantly.
Conclusion
The second heart sound (S2) is a critical indicator of cardiac function and health. By understanding its components, clinical significance, and the conditions affecting it, healthcare providers can make accurate diagnoses and provide effective treatments. Advances in diagnostic techniques, such as echocardiography and phonocardiography, have further enhanced our ability to evaluate S2, leading to better patient outcomes.
Understanding and interpreting the second heart sound is crucial for anyone involved in cardiac care. This knowledge helps in diagnosing various cardiac conditions and planning appropriate interventions, ultimately improving patient care and outcomes.
List of Diseases Related to the Second Heart Sound
See Also:
- Aortic Stenosis
- Pulmonary Hypertension
- Atrial Septal Defect
- Right Bundle Branch Block
- Left Bundle Branch Block
- Aortic Regurgitation
- Mitral Stenosis
- Mitral Regurgitation
- Systemic Hypertension
- Pulmonary Stenosis
- Hyperthyroidism
- Coarctation of the Aorta
- Chronic Obstructive Pulmonary Disease (COPD)
Read Also: First heart sound
References:
Yamaguchi, S., & Little, W. C. (2006). The Second Heart Sound. Circulation, 113(20), e652-e653. https://doi.org/10.1161/CIRCULATIONAHA.106.616300
Boettger, S., Hoyer, D., Falkenhain, K., Bär, K. J., & Voss, A. (2010). Heart rate variability and QT variability in male patients with depression. Journal of Affective Disorders, 124(1-2), 129-136. https://doi.org/10.1016/j.jad.2009.11.009
Frazer, C. A., & Stein, P. D. (2001). Murmurs, heart sounds, and physical diagnosis of the heart. Journal of the American College of Cardiology, 38(5), 1391. https://doi.org/10.1016/S0735-1097(01)01500-5
Perloff, J. K. (1984). The Clinical Recognition of Congenital Heart Disease. WB Saunders Co, 4th edition.
Libby, P., Bonow, R. O., Mann, D. L., & Zipes, D. P. (2007). Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. Elsevier Health Sciences.
Otto, C. M., & Bonow, R. O. (2012). Valvular Heart Disease: A Companion to Braunwald’s Heart Disease. Elsevier Health Sciences.
McGee, S. R. (2007). Evidence-Based Physical Diagnosis. Elsevier Health Sciences.
Mangione, S., & Nieman, L. Z. (1997). Cardiac auscultatory skills of internal medicine and family practice trainees. Journal of the American Medical Association, 278(9), 717-722. https://doi.org/10.1001/jama.1997.03550090047030
Bickley, L. S., & Szilagyi, P. G. (2009). Bates’ Guide to Physical Examination and History Taking. Lippincott Williams & Wilkins.
Waggoner, A. D., & Adyanthaya, A. V. (2008). Echocardiographic Assessment of Prosthetic Valves. Progress in Cardiovascular Diseases, 50(4), 245-268. https://doi.org/10.1016/j.pcad.2007.11.002
- Refererences:
- Yamaguchi, S., & Little, W. C. (2006). The Second Heart Sound. Circulation, 113(20), e652-e653. https://doi.org/10.1161/CIRCULATIONAHA.106.616300
- Boettger, S., Hoyer, D., Falkenhain, K., Bär, K. J., & Voss, A. (2010). Heart rate variability and QT variability in male patients with depression. Journal of Affective Disorders, 124(1-2), 129-136. https://doi.org/10.1016/j.jad.2009.11.009
- Frazer, C. A., & Stein, P. D. (2001). Murmurs, heart sounds, and physical diagnosis of the heart. Journal of the American College of Cardiology, 38(5), 1391. https://doi.org/10.1016/S0735-1097(01)01500-5
- Perloff, J. K. (1984). The Clinical Recognition of Congenital Heart Disease. WB Saunders Co, 4th edition.
- Libby, P., Bonow, R. O., Mann, D. L., & Zipes, D. P. (2007). Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. Elsevier Health Sciences.
- Otto, C. M., & Bonow, R. O. (2012). Valvular Heart Disease: A Companion to Braunwald’s Heart Disease. Elsevier Health Sciences.
- McGee, S. R. (2007). Evidence-Based Physical Diagnosis. Elsevier Health Sciences.
- Mangione, S., & Nieman, L. Z. (1997). Cardiac auscultatory skills of internal medicine and family practice trainees. Journal of the American Medical Association, 278(9), 717-722. https://doi.org/10.1001/jama.1997.03550090047030
- Bickley, L. S., & Szilagyi, P. G. (2009). Bates’ Guide to Physical Examination and History Taking. Lippincott Williams & Wilkins.
- Waggoner, A. D., & Adyanthaya, A. V. (2008). Echocardiographic Assessment of Prosthetic Valves. Progress in Cardiovascular Diseases, 50(4), 245-268. https://doi.org/10.1016/j.pcad.2007.11.002