Anatomy of the Human Heart: An In-Depth Exploration
Introduction
The human heart is a marvel of biological engineering, tirelessly pumping blood throughout our bodies to sustain life. Understanding its anatomy is crucial for comprehending how this vital organ functions. In this blog post, we will explore the structure of the human heart, breaking down its components and their roles in the circulatory system.
Outline
- Overview of the Heart
- Heart Chambers
- Right Atrium
- Right Ventricle
- Left Atrium
- Left Ventricle
- Heart Valves
- Tricuspid Valve
- Pulmonary Valve
- Mitral Valve
- Aortic Valve
- Blood Vessels
- Major Arteries
- Major Veins
- The Cardiac Conduction System
- Sinoatrial (SA) Node
- Atrioventricular (AV) Node
- Bundle of His
- Purkinje Fibers
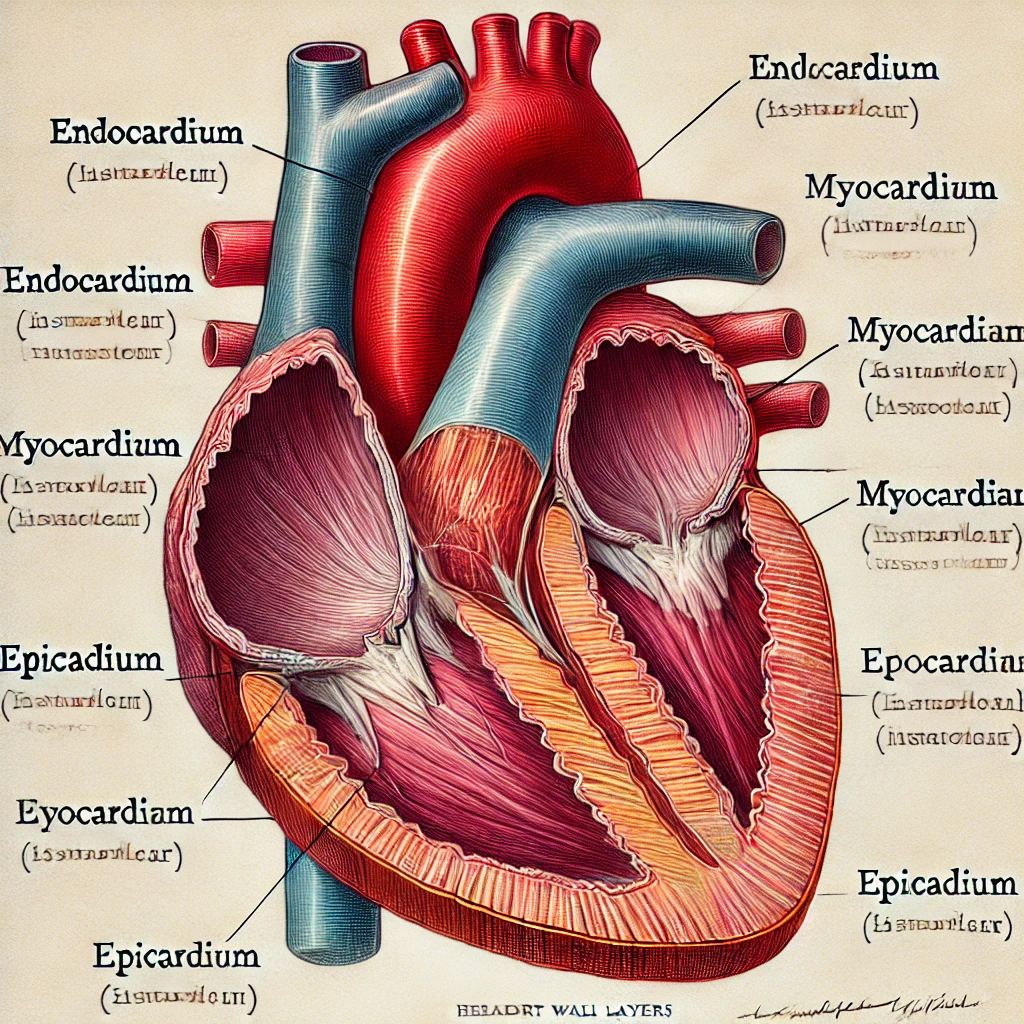
- Heart Wall Layers
- Endocardium
- Myocardium
- Epicardium
- Coronary Circulation
- Diseases of the Heart
- Conclusion
Overview of the Heart
The heart is a muscular organ located in the thoracic cavity, slightly to the left of the midline. It is about the size of a clenched fist and weighs between 250 to 350 grams. The primary function of the heart is to pump blood through the circulatory system, delivering oxygen and nutrients to tissues and removing waste products.
Structure and Function
The heart is composed of four main chambers: the right atrium, right ventricle, left atrium, and left ventricle. Blood flows through these chambers in a precise sequence, driven by the coordinated contraction of the heart muscle. The rhythmic contractions are regulated by the cardiac conduction system, ensuring that the heart beats consistently and effectively.
Blood vessels, including arteries and veins, are connected to the heart, forming a complex network that transports blood to and from all parts of the body. The coronary arteries specifically supply the heart muscle with oxygen-rich blood, essential for its functioning.
Role in Circulatory System
The heart’s role in the circulatory system is vital for maintaining homeostasis. It ensures that oxygen-depleted blood is sent to the lungs for oxygenation and that oxygen-rich blood is distributed to the rest of the body. This dual-pump system is efficient and robust, capable of adjusting to varying physiological demands, such as during exercise or stress.
Protective Structures
Structurally, the heart is enclosed within the pericardium, a double-walled sac that provides protection and reduces friction as the heart beats. The inner layer of the pericardium, the serous pericardium, produces a lubricating fluid that further minimizes friction.
Endocrine Function
In addition to its mechanical functions, the heart also plays a role in endocrine signaling. The atria produce a hormone called atrial natriuretic peptide (ANP), which helps regulate blood pressure by promoting the excretion of sodium and water by the kidneys.
Importance in Medicine
Understanding the detailed anatomy and function of the heart is essential for diagnosing and treating cardiovascular diseases, which remain a leading cause of morbidity and mortality worldwide. Advances in medical imaging, such as echocardiography and MRI, have significantly enhanced our ability to visualize and understand heart structure and function, leading to better diagnostic and therapeutic strategies.
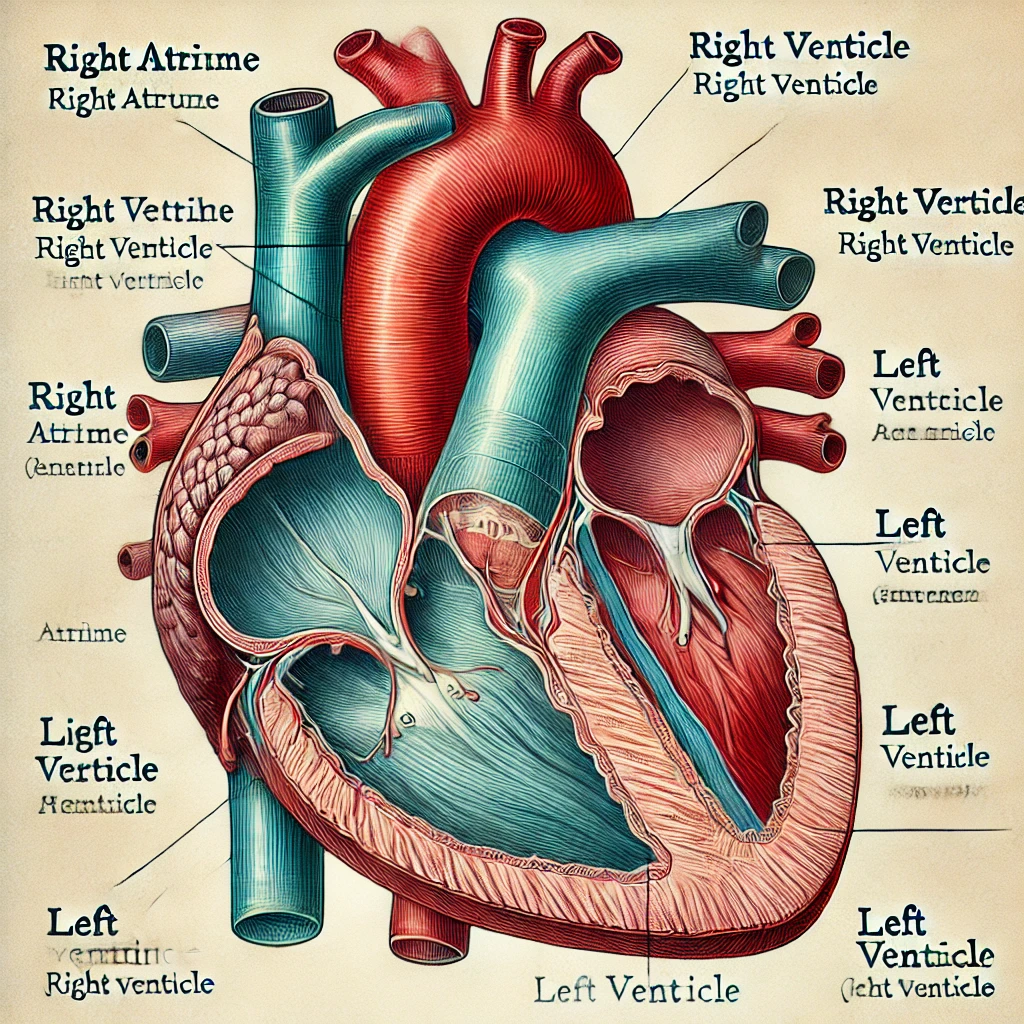
Heart Chambers
The heart’s four chambers play distinct yet interrelated roles in circulating blood throughout the body. Each chamber has a specific function and is structurally adapted to optimize its role in the circulatory process.
Right Atrium
The right atrium is one of the two upper chambers of the heart. It receives deoxygenated blood from the body through the superior and inferior vena cavae. The right atrium serves as a reservoir, holding blood until it can be pumped into the right ventricle. This chamber also contains the sinoatrial (SA) node, often referred to as the heart’s natural pacemaker. The SA node generates electrical impulses that initiate each heartbeat, causing the atria to contract and pump blood into the ventricles. The presence of the SA node in the right atrium is crucial for maintaining a regular and coordinated heartbeat.
Right Ventricle
The right ventricle receives blood from the right atrium and pumps it to the lungs via the pulmonary artery for oxygenation. The walls of the right ventricle are thinner than those of the left ventricle because it only needs to pump blood a short distance to the lungs. The right ventricle’s structure is optimized for this lower-pressure task, ensuring efficient pulmonary circulation. The right ventricle’s function is supported by the tricuspid valve, which prevents backflow of blood into the right atrium during ventricular contraction.
Left Atrium
The left atrium receives oxygenated blood from the lungs through the pulmonary veins. Like the right atrium, it serves as a holding chamber, allowing blood to accumulate before being pumped into the left ventricle. The left atrium’s walls are slightly thicker than those of the right atrium to accommodate the increased pressure of oxygenated blood. The mitral valve, also known as the bicuspid valve, is situated between the left atrium and left ventricle, preventing backflow during ventricular contraction.
Left Ventricle
The left ventricle is the most muscular chamber of the heart, responsible for pumping oxygenated blood to the rest of the body through the aorta. Its thick walls generate the high pressure needed to propel blood through the systemic circulation, ensuring that all tissues receive an adequate supply of oxygen and nutrients. The left ventricle’s powerful contractions are essential for maintaining effective blood flow throughout the body. The aortic valve, located between the left ventricle and the aorta, ensures that blood flows efficiently into the systemic circulation without backflow.
Coordinated Function
Each chamber of the heart plays a vital role in maintaining the continuous flow of blood, with valves ensuring that blood moves in the correct direction and does not flow backward. The coordinated function of the atria and ventricles ensures efficient circulation, supporting the body’s metabolic needs. Understanding the structure and function of each heart chamber is essential for diagnosing and treating cardiovascular conditions, such as atrial fibrillation, ventricular hypertrophy, and heart failure.
By appreciating the unique roles and adaptations of the heart’s chambers, we gain insight into the intricate design and function of this vital organ. The following sections will further explore the specific structures that support the heart’s function, including the valves, blood vessels, and conduction system.
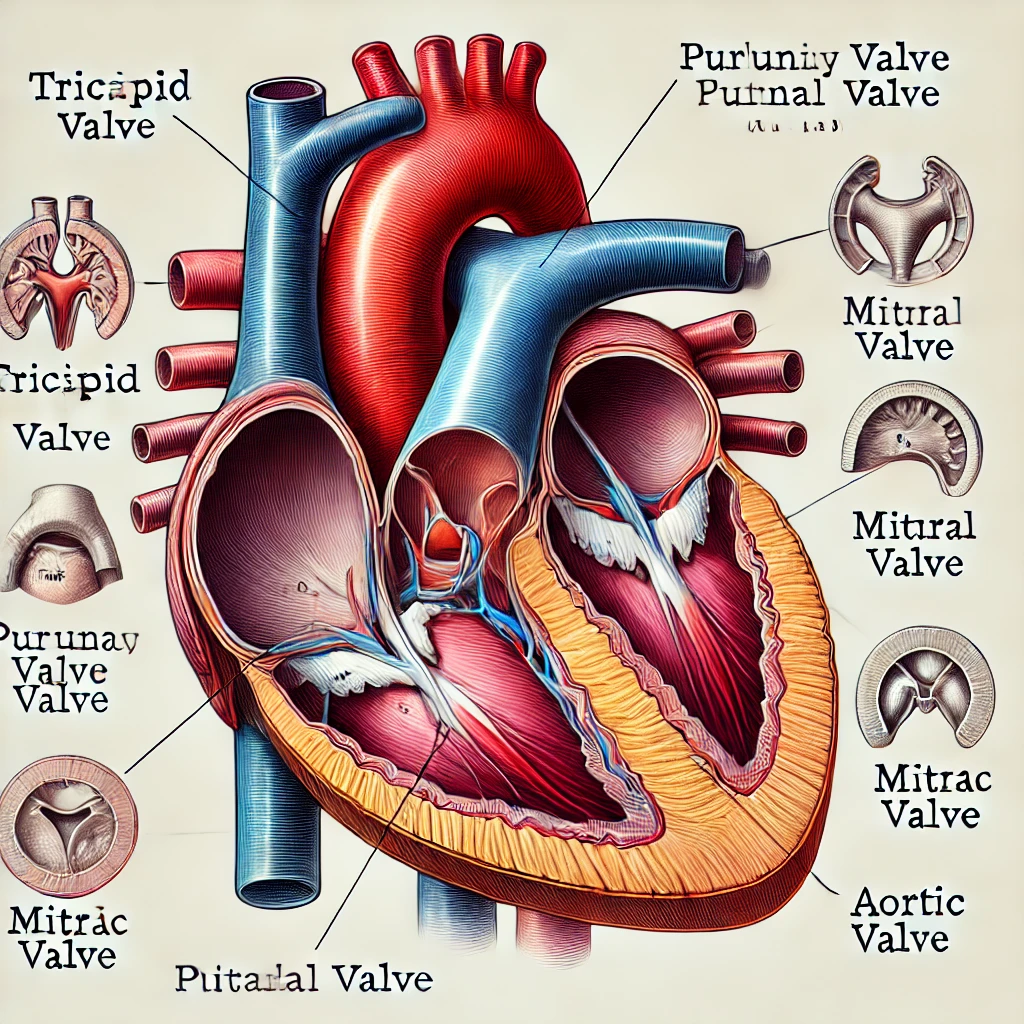
Heart Valves
Valves are crucial in maintaining unidirectional blood flow through the heart, preventing backflow and ensuring efficient circulation. Each valve is strategically located to regulate the flow of blood between the heart’s chambers and major blood vessels.
Tricuspid Valve
The tricuspid valve is located between the right atrium and right ventricle. It consists of three cusps (or leaflets) that open to allow blood to flow from the right atrium into the right ventricle and close to prevent backflow when the ventricle contracts. The tricuspid valve’s structure is designed to withstand the pressures exerted during ventricular contraction, ensuring a tight seal that prevents regurgitation.
Pulmonary Valve
Situated between the right ventricle and the pulmonary artery, the pulmonary valve prevents backflow of blood into the right ventricle after it has been pumped into the pulmonary artery. This valve has three cusps and operates similarly to the tricuspid valve. The pulmonary valve’s function is essential for maintaining efficient pulmonary circulation, directing deoxygenated blood to the lungs for oxygenation.
Mitral Valve
Also known as the bicuspid valve, the mitral valve is located between the left atrium and left ventricle. It has two cusps that function like doors, opening to allow blood to flow from the left atrium into the left ventricle and closing to prevent backflow during ventricular contraction. The mitral valve’s design is optimized for the high-pressure environment of the left ventricle, ensuring that oxygenated blood is efficiently directed into the systemic circulation.
Aortic Valve
The aortic valve is located between the left ventricle and the aorta. It prevents blood from flowing back into the left ventricle after it has been pumped into the aorta. Like the pulmonary valve, the aortic valve has three cusps and ensures that blood moves efficiently into the systemic circulation. The aortic valve’s
function is critical for maintaining the unidirectional flow of blood, supporting the heart’s role in delivering oxygen and nutrients to the body’s tissues.
Function and Disorders
Each valve’s precise opening and closing are critical for the heart’s function, coordinating the timing of blood flow to maximize efficiency and maintain proper circulation. Valve disorders, such as stenosis or regurgitation, can significantly impact heart function, leading to symptoms such as shortness of breath, fatigue, and chest pain. Understanding the structure and function of heart valves is essential for diagnosing and treating these conditions, ensuring that the heart continues to function effectively.
Advances in medical technology, such as echocardiography and cardiac MRI, have enhanced our ability to visualize and assess valve function, leading to improved diagnostic and therapeutic strategies. Surgical and minimally invasive techniques, such as valve replacement and repair, have also advanced, offering effective treatment options for valve disorders. By appreciating the intricate design and function of heart valves, we gain insight into the heart’s overall efficiency and resilience, highlighting the importance of maintaining cardiovascular health.
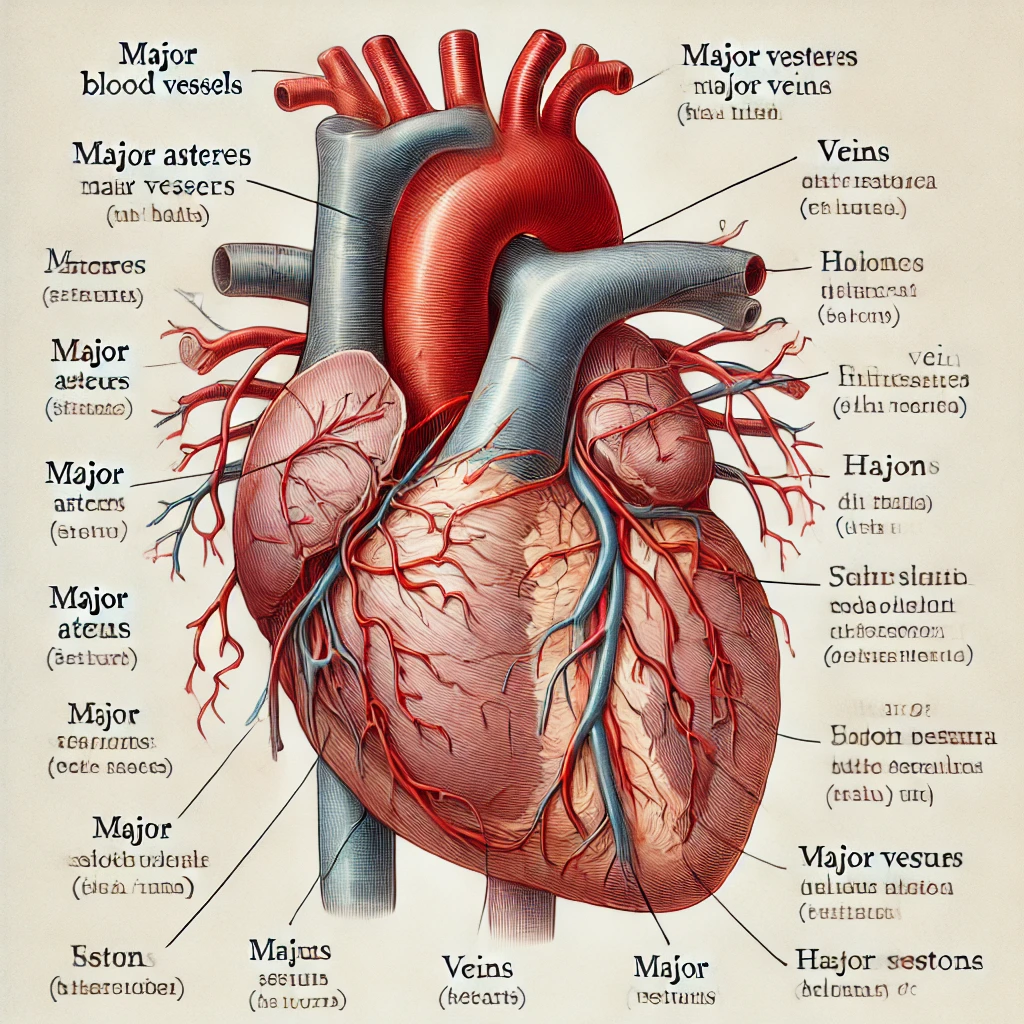
Blood Vessels
Blood vessels are the conduits through which blood travels, with arteries carrying oxygenated blood away from the heart and veins returning deoxygenated blood to the heart. These vessels form a complex network that supports the circulatory system’s function, ensuring that all tissues receive an adequate supply of oxygen and nutrients.
Major Arteries
- Aorta: The largest artery in the body, the aorta carries oxygenated blood from the left ventricle to all parts of the body. It branches into smaller arteries that distribute blood to various organs and tissues. The aorta’s structure is designed to withstand the high pressure generated by the left ventricle’s contractions, ensuring efficient systemic circulation.
- Pulmonary Artery: This artery carries deoxygenated blood from the right ventricle to the lungs for oxygenation. It splits into the left and right pulmonary arteries, each leading to the corresponding lung. The pulmonary artery‘s function is essential for maintaining effective pulmonary circulation, supporting the exchange of oxygen and carbon dioxide in the lungs.
Major Veins
- Superior and Inferior Vena Cavae: These veins return deoxygenated blood from the body to the right atrium. The superior vena cava drains blood from the upper body, while the inferior vena cava drains blood from the lower body. The vena cavae’s function is crucial for maintaining the return flow of blood to the heart, ensuring continuous circulation.
- Pulmonary Veins: These veins carry oxygenated blood from the lungs to the left atrium. There are four pulmonary veins, two from each lung, ensuring a steady supply of oxygenated blood to the heart. The pulmonary veins’ function is essential for supporting systemic circulation, delivering oxygen-rich blood to the body’s tissues.
Function and Disorders
The efficient functioning of these blood vessels is vital for maintaining the circulation of blood, ensuring that oxygen and nutrients are delivered to tissues while waste products are removed. Blood vessel disorders, such as atherosclerosis and aneurysms, can significantly impact cardiovascular health, leading to complications such as heart attack, stroke, and peripheral artery disease. Understanding the structure and function of blood vessels is essential for diagnosing and treating these conditions, ensuring that the circulatory system continues to function effectively.
Advances in medical technology, such as angiography and ultrasound, have enhanced our ability to visualize and assess blood vessel function, leading to improved diagnostic and therapeutic strategies. Interventional techniques, such as angioplasty and stent placement, have also advanced, offering effective treatment options for blood vessel disorders. By appreciating the intricate design and function of blood vessels, we gain insight into the circulatory system’s overall efficiency and resilience, highlighting the importance of maintaining cardiovascular health.
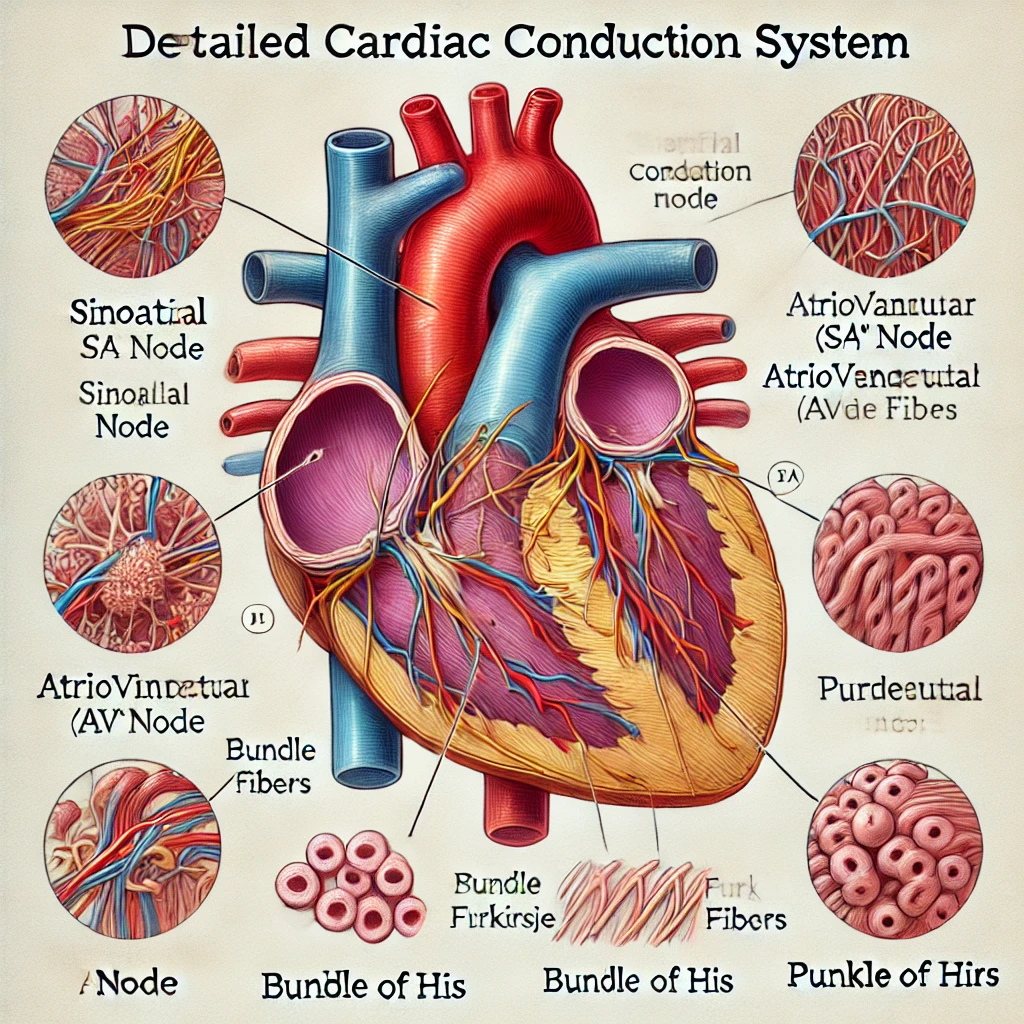
The Cardiac Conduction System
The cardiac conduction system is responsible for controlling the heart rate and coordinating the contraction of the heart chambers. This system ensures that the heart beats in a regular and synchronized manner, maintaining efficient circulation.
Sinoatrial (SA) Node
The SA node, located in the right atrium, is the heart’s natural pacemaker. It generates electrical impulses that initiate each heartbeat, causing the atria to contract and pump blood into the ventricles. The SA node’s function is essential for maintaining a regular and coordinated heartbeat, ensuring that the heart functions effectively.
Atrioventricular (AV) Node
Located between the atria and ventricles, the AV node receives impulses. from the SA node and relays them to the ventricles. It also provides a brief delay, allowing the ventricles to fill with blood before they contract. The AV node’s function is crucial for maintaining the coordination of atrial and ventricular contractions, ensuring efficient circulation.
Bundle of His
The Bundle of His transmits electrical impulses from the AV node to the ventricles through the interventricular septum. It divides into left and right bundle branches, which carry the impulses to the respective ventricles. The Bundle of His’s function is essential for maintaining the coordination of ventricular contractions, ensuring efficient circulation.
Purkinje Fibers
These fibers distribute the electrical impulse throughout the ventricles, causing them to contract and pump blood to the lungs and the rest of the body. The Purkinje fibers’ function is crucial for maintaining the coordination of ventricular contractions, ensuring efficient circulation.
Function and Disorders
The precise timing of electrical impulses ensures that the heart beats in a coordinated and efficient manner, maintaining a regular rhythm and effective circulation. Disorders of the cardiac conduction system, such as arrhythmias and heart block, can significantly impact heart function, leading to symptoms such as palpitations, dizziness, and syncope. Understanding the structure and function of the cardiac conduction system is essential for diagnosing and treating these conditions, ensuring that the heart continues to function effectively.
Advances in medical technology, such as electrocardiography (ECG) and electrophysiology studies, have enhanced our ability to visualize and assess the function of the cardiac conduction system, leading to improved diagnostic and therapeutic strategies. Interventional techniques, such as pacemaker implantation and ablation, have also advanced, offering effective treatment options for conduction system disorders. By appreciating the intricate design and function of the cardiac conduction system, we gain insight into the heart’s overall efficiency and resilience, highlighting the importance of maintaining cardiovascular health.
Heart Wall Layers
The heart wall is composed of three layers, each with a specific function. These layers work together to ensure the heart’s structural integrity and functionality.
Endocardium
The innermost layer, the endocardium lines the heart chambers and valves. It is composed of endothelial cells and provides a smooth surface for blood to flow over, minimizing friction and preventing clot formation. The endocardium’s function is essential for maintaining the integrity of the heart’s internal structures, supporting efficient circulation.
Myocardium
The myocardium is the thick, muscular middle layer responsible for the heart’s contractile force. It is composed of cardiac muscle cells (myocytes) that contract to pump blood. The myocardium is thicker in the left ventricle than in the right ventricle, reflecting the greater force needed to pump blood through the systemic circulation. The myocardium’s function is crucial for maintaining the heart’s pumping ability, supporting efficient circulation.
Epicardium
The epicardium is the outermost layer of the heart wall, forming part of the pericardium, which surrounds and protects the heart. It contains connective tissue, fat, and blood vessels that supply the heart muscle with oxygen and nutrients. The epicardium’s function is essential for maintaining the heart’s structural integrity and supporting efficient circulation.
Function and Disorders
Together, these layers work in harmony to ensure the heart’s structural integrity and functionality. Disorders of the heart wall, such as myocarditis and endocarditis, can significantly impact heart function, leading to symptoms such as chest pain, fatigue, and heart failure. Understanding the structure and function of the heart wall is essential for diagnosing and treating these conditions, ensuring that the heart continues to function effectively.
Advances in medical technology
, such as cardiac MRI and echocardiography, have enhanced our ability to visualize and assess the structure and function of the heart wall, leading to improved diagnostic and therapeutic strategies. Surgical and minimally invasive techniques, such as valve replacement and repair, have also advanced, offering effective treatment options for heart wall disorders. By appreciating the intricate design and function of the heart wall, we gain insight into the heart’s overall efficiency and resilience, highlighting the importance of maintaining cardiovascular health.
Coronary Circulation
The heart has its own blood supply through the coronary arteries and veins, ensuring that it receives the oxygen and nutrients needed to function effectively. Efficient coronary circulation is essential for maintaining the heart’s health and preventing conditions such as myocardial infarction (heart attack).
Coronary Arteries
The right and left coronary arteries branch from the aorta and supply oxygen-rich blood to the heart muscle. The left coronary artery further divides into the left anterior descending artery and the circumflex artery, each supplying different regions of the heart. The coronary arteries’ function is crucial for maintaining the heart’s health and supporting efficient circulation.
Cardiac Veins
The cardiac veins collect deoxygenated blood from the heart muscle and return it to the right atrium. Major cardiac veins include the great cardiac vein, middle cardiac vein, and small cardiac vein, which drain into the coronary sinus. The cardiac veins’ function is essential for maintaining the return flow of blood to the heart, ensuring continuous circulation.
Function and Disorders
Efficient coronary circulation is essential for maintaining the heart’s health and preventing conditions such as myocardial infarction (heart attack). Understanding the structure and function of coronary circulation is essential for diagnosing and treating these conditions, ensuring that the heart continues to function effectively.
Advances in medical technology, such as coronary angiography and CT angiography, have enhanced our ability to visualize and assess the structure and function of coronary circulation, leading to improved diagnostic and therapeutic strategies. Interventional techniques, such as angioplasty and stent placement, have also advanced, offering effective treatment options for coronary artery disease. By appreciating the intricate design and function of coronary circulation, we gain insight into the heart’s overall efficiency and resilience, highlighting the importance of maintaining cardiovascular health.
Diseases of the Heart
The heart can be affected by a wide range of diseases, which can significantly impact its function and the overall health of the individual. These diseases can be broadly categorized into congenital, structural, electrical, and vascular conditions.
Congenital Heart Diseases
- Congenital Heart Defects: These are structural problems present at birth, affecting the heart’s chambers, valves, or blood vessels. Examples include atrial septal defect, ventricular septal defect, and tetralogy of Fallot.
Structural Heart Diseases
- Cardiomyopathy: This refers to diseases of the heart muscle that make it harder for the heart to pump blood to the rest of the body. Examples include dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy.
- Heart Valve Disease: Conditions affecting the function of the heart valves, such as aortic stenosis and mitral valve prolapse, can lead to disrupted blood flow within the heart.
Electrical Heart Diseases
- Arrhythmias: These are disorders of the heart rate or rhythm, such as atrial fibrillation, ventricular tachycardia, and heart block.
- Long QT Syndrome: This is a condition that affects the heart’s electrical activity, leading to sudden, uncontrollable, and dangerous heart rhythms.
Vascular Heart Diseases
- Coronary Artery Disease: This is the most common type of heart disease, caused by the buildup of plaque in the coronary arteries, leading to reduced blood flow to the heart muscle. It can result in angina and myocardial infarction.
- Hypertension: High blood pressure can lead to damage to the heart and blood vessels over time, increasing the risk of heart disease and stroke.
Inflammatory Heart Diseases
- Myocarditis: Inflammation of the heart muscle, often caused by viral infections, can lead to heart dysfunction.
- Endocarditis: Infection of the inner lining of the heart chambers and valves, typically caused by bacteria, can damage the heart and lead to serious complications.
- Pericarditis: Inflammation of the pericardium, the protective sac surrounding the heart, can cause chest pain and other symptoms.
Metabolic Heart Diseases
- Diabetic Cardiomyopathy: Diabetes can lead to changes in the heart muscle, increasing the risk of heart failure.
- Hyperlipidemia: High levels of lipids (fats) in the blood, such as cholesterol, can contribute to the development of atherosclerosis and coronary artery disease.
Impact and Management
The impact of heart disease on health can be profound, leading to reduced quality of life, disability, and premature death. management of heart disease typically involves lifestyle changes, medications, and sometimes surgical interventions. Regular monitoring and early detection are crucial for effective treatment and management of heart conditions.
Advances in medical research and technology continue to improve our understanding of heart diseases and the development of new treatments. Public health initiatives aimed at promoting heart-healthy lifestyles and reducing risk factors, such as smoking and poor diet, play a vital role in preventing heart disease.
Conclusion
Understanding the anatomy of the human heart reveals the complexity and efficiency of this vital organ. Each component plays a crucial role in maintaining the circulatory system, ensuring that our bodies receive the oxygen and nutrients needed for survival. As we continue to explore and study the heart, we gain deeper insights into its function and ways to maintain its health.
By grasping the intricacies of heart anatomy, we can better appreciate the importance of cardiovascular health and the advances in medical science that help us care for this essential organ.




