Introduction
Coronary Artery Disease (CAD) is a significant medical condition affecting millions of people worldwide. It is the most common type of heart disease and a leading cause of death. Understanding CAD is crucial for preventing and managing this life-threatening condition. In this blog post, we will explore what CAD is, its causes, symptoms, diagnosis, treatment options, prevention strategies, and tips for living with CAD.
What is Coronary Artery Disease (CAD)?
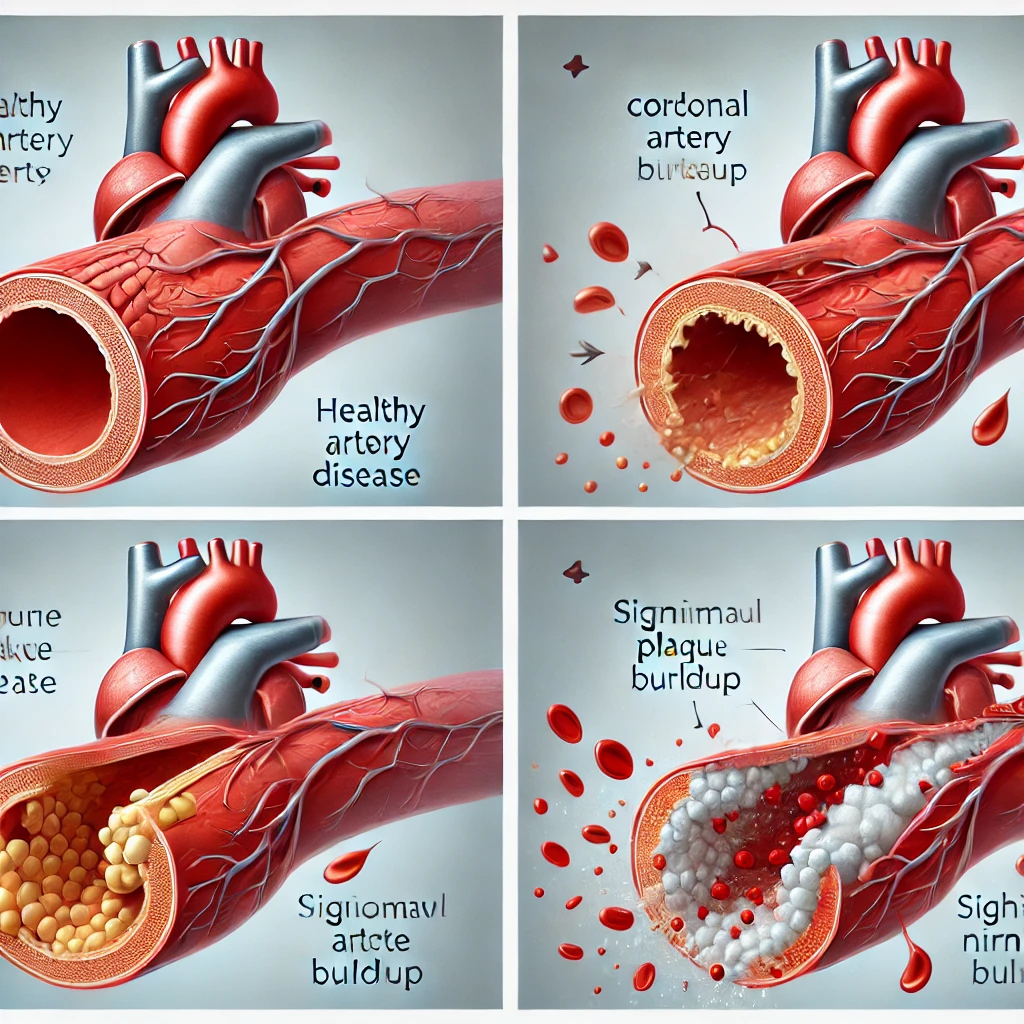
Definition and Mechanism
Coronary Artery Disease (CAD) occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked. This is primarily due to a buildup of plaque, a substance made up of fat, cholesterol, and other cellular waste products. This process is known as atherosclerosis. Over time, the plaque hardens, narrowing the arteries and reducing blood flow to the heart. This reduced blood flow can lead to chest pain (angina), shortness of breath, or other symptoms. In severe cases, it can result in a heart attack.
Statistics and Impact
CAD is a prevalent condition. According to the World Health Organization (WHO), it is responsible for approximately 17.9 million deaths each year, accounting for 31% of all global deaths. The burden of CAD is significant, affecting not only the individuals with the disease but also their families and healthcare systems worldwide.
Pathophysiology
The pathophysiology of CAD involves complex interactions between genetic, environmental, and lifestyle factors. The disease process begins with damage to the inner layer of a coronary artery. This damage may be caused by various factors, including high blood pressure, high cholesterol, smoking, diabetes, and other risk factors. Once the artery is damaged, cholesterol and other substances in the bloodstream accumulate at the site of injury, forming a plaque. Over time, this plaque can harden and narrow the artery, reducing blood flow to the heart.
When the blood flow is reduced, the heart muscle does not get enough oxygen, leading to symptoms such as chest pain and shortness of breath. In some cases, the plaque can rupture, causing a blood clot to form. If the clot becomes large enough, it can completely block the flow of blood through the artery, resulting in a heart attack.
Types of Coronary Artery Disease
There are several types of CAD, each with its own characteristics and implications:
- Stable Angina: This type of angina occurs predictably with exertion or emotional stress and is relieved by rest or medication.
- Unstable Angina: This type of angina occurs unpredictably, often at rest, and is not relieved by rest or medication. It is a medical emergency as it can precede a heart attack.
- Variant (Prinzmetal’s) Angina: This type of angina is caused by a spasm in the coronary arteries and can occur at rest.
- Microvascular Angina: This type involves the small coronary arteries (microvasculature) and may cause angina-like symptoms despite normal major coronary arteries.

Causes and Risk Factors
Atherosclerosis and Plaque Buildup
The primary cause of CAD is atherosclerosis, a condition characterized by the buildup of plaque within the coronary arteries. This plaque consists of cholesterol, fatty substances, cellular waste products, calcium, and fibrin, a clotting material in the blood. As the plaque accumulates, the arteries narrow, limiting the flow of oxygen-rich blood to the heart.
Major Risk Factors
Several factors contribute to the development of CAD. Understanding these risk factors can help in prevention and management:
- High Blood Pressure (Hypertension): Increased pressure on the arterial walls can damage them, promoting plaque buildup.
- High Cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol can lead to plaque formation.
- Smoking: Tobacco use damages the blood vessels and accelerates the development of atherosclerosis.
- Diabetes: High blood sugar levels can damage blood vessels and contribute to CAD.
- Obesity: Excess weight often leads to other risk factors such as hypertension, diabetes, and high cholesterol.
- Sedentary Lifestyle: Lack of physical activity can increase the risk of CAD.
- Family History: Genetics play a role in the susceptibility to CAD.
- Age and Gender: The risk increases with age, and men are generally at higher risk, although the risk for women increases post-menopause.
Secondary Risk Factors
In addition to the primary risk factors, other conditions such as stress, excessive alcohol consumption, and an unhealthy diet can also contribute to the development of CAD. It is essential to manage these risk factors through lifestyle changes and medical intervention.
Genetic Predisposition
Genetics play a crucial role in the development of CAD. Certain genetic factors can influence cholesterol levels, blood pressure, and the body’s ability to process fats. Individuals with a family history of heart disease are at a higher risk of developing CAD. Research is ongoing to identify specific genetic markers that can predict the likelihood of CAD and help in early detection and prevention.
Environmental Factors
Environmental factors, including air pollution and exposure to secondhand smoke, can also contribute to the development of CAD. Studies have shown that long-term exposure to air pollution can increase the risk of heart disease. Efforts to reduce environmental pollutants and promote clean air can help mitigate this risk.
Lifestyle Factors
Lifestyle choices significantly impact the risk of developing CAD. Here are some critical lifestyle factors:
- Diet: A diet high in saturated fats, trans fats, and cholesterol can contribute to plaque buildup in the arteries. Conversely, a diet rich in fruits, vegetables, whole grains, and lean proteins can help protect against CAD.
- Physical Activity: Regular exercise helps maintain a healthy weight, reduces blood pressure, improves cholesterol levels, and reduces stress, all of which can lower the risk of CAD.
- Alcohol Consumption: Excessive alcohol intake can raise blood pressure and contribute to heart disease. Moderation is key, with some studies suggesting that moderate alcohol consumption may have a protective effect on the heart.
Managing Risk Factors
Effective management of risk factors involves a combination of lifestyle changes and medical treatments. Regular check-ups and screenings can help detect risk factors early and allow for timely intervention. Here are some strategies for managing risk factors:
- Dietary Changes: Adopting a heart-healthy diet that is low in saturated fats, trans fats, cholesterol, and sodium can help reduce the risk of CAD. Incorporating more fruits, vegetables, whole grains, and lean proteins is beneficial.
- Regular Exercise: Engaging in at least 150 minutes of moderate-intensity exercise per week can improve cardiovascular health and reduce risk factors.
- Smoking Cessation: Quitting smoking is one of the most significant steps in reducing the risk of CAD. Various cessation programs, medications, and support groups can help individuals quit smoking.
- Weight Management: Achieving and maintaining a healthy weight through diet and exercise can help control other risk factors such as diabetes and hypertension.
- Stress Management: Practicing stress-reducing techniques such as meditation, yoga, and deep breathing can improve overall heart health.
- Regular Health Screenings: Routine check-ups and screenings for blood pressure, cholesterol, and diabetes can help detect and manage risk factors early.
Symptoms of Coronary Artery Disease
Common Symptoms
The symptoms of CAD can vary from mild to severe and may develop gradually over time. Some common symptoms include:
- Chest Pain (Angina): This is the most common symptom. It may feel like pressure, tightness, or squeezing in the chest. Angina can also radiate to the shoulders, arms, neck, jaw, or back.
- Shortness of Breath: Reduced blood flow to the heart can cause difficulty breathing, especially during physical activity.
- Fatigue: A decrease in oxygen supply to the heart can lead to feelings of tiredness and weakness.
Warning Signs of a Heart Attack
A heart attack occurs when a coronary artery becomes completely blocked, cutting off the blood supply to part of the heart muscle. The following symptoms may indicate a heart attack:
- Severe Chest Pain: Persistent pain that doesn’t go away with rest.
- Pain in the Upper Body: Discomfort or pain in the arms, neck, jaw, back, or stomach.
- Nausea or Vomiting: Feeling sick to the stomach or actual vomiting.
- Sweating: Breaking out in a cold sweat without apparent reason.
- Lightheadedness: Feeling dizzy or faint.
Atypical Symptoms
Some individuals, especially women, the elderly, and those with diabetes, may experience atypical symptoms such as indigestion, heartburn, or upper back pain. It is important to recognize these less obvious signs and seek medical attention if they occur.
Silent Ischemia
Silent ischemia is a condition where the heart does not receive enough oxygen, but the individual does not experience any noticeable symptoms. This condition can be dangerous as it can lead to a heart attack without warning. Regular check-ups and diagnostic tests are essential for detecting silent ischemia.
Angina Pectoris
It is chest pain caused by reduced blood flow to the heart muscle. It is a symptom of CAD and can be classified into different types:
- Stable Angina: Occurs predictably with exertion or stress and is relieved by rest or medication.
- Unstable Angina: Occurs unpredictably, often at rest, and is not relieved by rest or medication. It is a medical emergency as it can precede a heart attack.
- Variant (Prinzmetal’s) Angina: Caused by a spasm in the coronary arteries and can occur at rest.
- Microvascular Angina: Involves the small coronary arteries (microvasculature) and may cause angina-like symptoms despite normal major coronary arteries.
Recognizing Symptoms Early
Early recognition of CAD symptoms is crucial for preventing complications. Here are some tips for recognizing symptoms:
- Pay Attention to Chest Discomfort: Any unusual chest discomfort, pressure, or pain should be evaluated by a healthcare professional.
- Monitor Breathing: Difficulty breathing during physical activity or at rest can be a sign of CAD.
- Notice Changes in Energy Levels: Unexplained fatigue or weakness can indicate reduced blood flow to the heart.
- Be Aware of Atypical Symptoms: Symptoms such as indigestion, heartburn, or upper back pain should not be ignored, especially in high-risk individuals.
When to Seek Medical Help
It is essential to seek medical help if you experience any symptoms of CAD, especially if they are severe or persistent. Here are some guidelines for when to seek medical help:
- Severe Chest Pain: Any severe or persistent chest pain should be evaluated immediately, as it may indicate a heart attack.
- Shortness of Breath: Difficulty breathing, especially if it occurs suddenly or without exertion, requires prompt medical attention.
- Fainting or Lightheadedness: Feeling faint or dizzy can be a sign of reduced blood flow to the brain and should be evaluated.
- Unexplained Symptoms: Any unexplained symptoms such as nausea, sweating, or upper body pain should be investigated.
Emergency Response
If you or someone else experiences symptoms of a heart attack, it is crucial to act quickly. Here are the steps to take in an emergency:
- Call Emergency Services: Dial emergency services immediately if you suspect a heart attack.
- Administer Aspirin: If the person is not allergic to aspirin and is conscious, they can chew a regular-strength aspirin to help prevent blood clotting.
- Use CPR if Necessary: If the person loses consciousness and is not breathing, perform CPR until emergency services arrive.
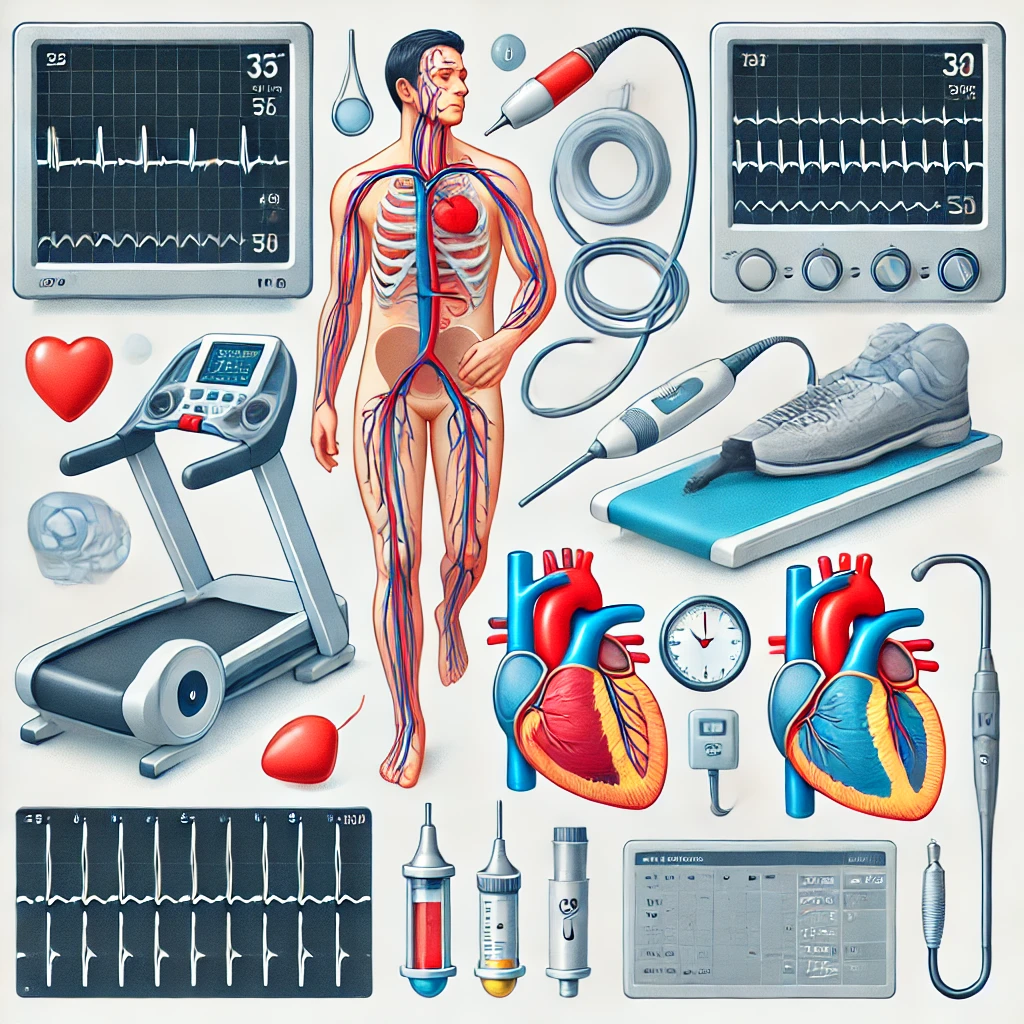
Diagnosis of CAD
Initial Evaluation
Diagnosing CAD typically begins with a thorough medical history and physical examination. During the evaluation, the doctor will assess risk factors, symptoms, and family history of heart disease. This initial assessment helps in determining the need for further diagnostic tests.
Diagnostic Procedures
Several tests are used to diagnose CAD and assess its severity:
- Electrocardiogram (EKG): This test records the electrical activity of the heart and can detect abnormalities that suggest CAD.
- Blood Tests: These tests measure cholesterol levels, blood sugar, and other markers that indicate heart health.
- Stress Testing: This involves exercising on a treadmill or stationary bike while monitoring the heart’s activity. It helps to determine how well the heart functions under stress.
- Echocardiogram: This ultrasound test provides images of the heart’s structure and function, helping to identify areas of poor blood flow or damage.
- Coronary Angiography: This invasive test involves injecting a contrast dye into the coronary arteries and taking X-ray images. It allows for visualization of blockages or narrowing in the arteries.
- CT Angiography: A non-invasive imaging test that provides detailed pictures of the coronary arteries using a CT scanner.
Interpreting Results
The results of these tests help doctors determine the presence and extent of CAD. Based on the findings, a personalized treatment plan can be developed to manage the condition effectively.
Advanced Diagnostic Techniques
In addition to the standard diagnostic procedures, advanced techniques are available for a more detailed assessment of CAD:
- Cardiac MRI: This imaging technique provides detailed images of the heart and can assess the extent of damage to the heart muscle.
- Intravascular Ultrasound (IVUS): This technique involves inserting a small ultrasound probe into the coronary arteries to provide detailed images of the artery walls and plaque buildup.
- Fractional Flow Reserve (FFR): This invasive procedure measures the pressure differences across a coronary artery stenosis to assess the severity of the blockage and guide treatment decisions.
Non-Invasive Tests
Non-invasive tests are often the first step in diagnosing CAD, providing valuable information without the need for invasive procedures:
- Electrocardiogram (EKG): This test records the electrical activity of the heart and can detect abnormalities that suggest CAD.
- Echocardiogram: This ultrasound test provides images of the heart’s structure and function, helping to identify areas of poor blood flow or damage.
- Stress Testing: This involves exercising on a treadmill or stationary bike while monitoring the heart’s activity. It helps to determine how well the heart functions under stress.
- CT Angiography: A non-invasive imaging test that provides detailed pictures of the coronary arteries using a CT scanner.
Invasive Tests
Invasive tests provide more detailed information about the coronary arteries and are typically performed when non-invasive tests suggest significant CAD:
- Coronary Angiography: This test involves injecting a contrast dye into the coronary arteries and taking X-ray images. It allows for visualization of blockages or narrowing in the arteries.
- Intravascular Ultrasound (IVUS): This technique involves inserting a small ultrasound probe into the coronary arteries to provide detailed images of the artery walls and plaque buildup.
- Fractional Flow Reserve (FFR): This procedure measures the pressure differences across a coronary artery stenosis to assess the severity of the blockage and guide treatment decisions.
Diagnosis of Coronary Artery Disease (CAD)
Risk Assessment Tools
Risk assessment tools help evaluate an individual’s risk of developing CAD and guide preventive measures:
- Framingham Risk Score: This tool estimates the 10-year risk of developing CAD based on factors such as age, gender, cholesterol levels, blood pressure, smoking status, and diabetes.
- Reynolds Risk Score: This score assesses the risk of CAD in women and includes factors such as age, cholesterol levels, blood pressure, smoking status, and high-sensitivity C-reactive protein (hs-CRP) levels.
- Atherosclerotic Cardiovascular Disease (ASCVD) Risk Calculator: This calculator estimates the 10-year risk of atherosclerotic cardiovascular disease, including CAD, based on factors such as age, gender, cholesterol levels, blood pressure, smoking status, diabetes, and use of blood pressure medications.
Importance of Early Diagnosis
Early diagnosis of CAD is crucial for preventing complications and improving outcomes. Here are some reasons why early diagnosis is important:
- Preventing Heart Attacks: Early detection and treatment of CAD can reduce the risk of heart attacks.
- Improving Quality of Life: Managing CAD early can improve symptoms and enhance the quality of life.
- Reducing Healthcare Costs: Early intervention can prevent costly complications and hospitalizations.
- Guiding Treatment Decisions: Early diagnosis allows for timely and appropriate treatment, reducing the progression of the disease.
Treatment Options
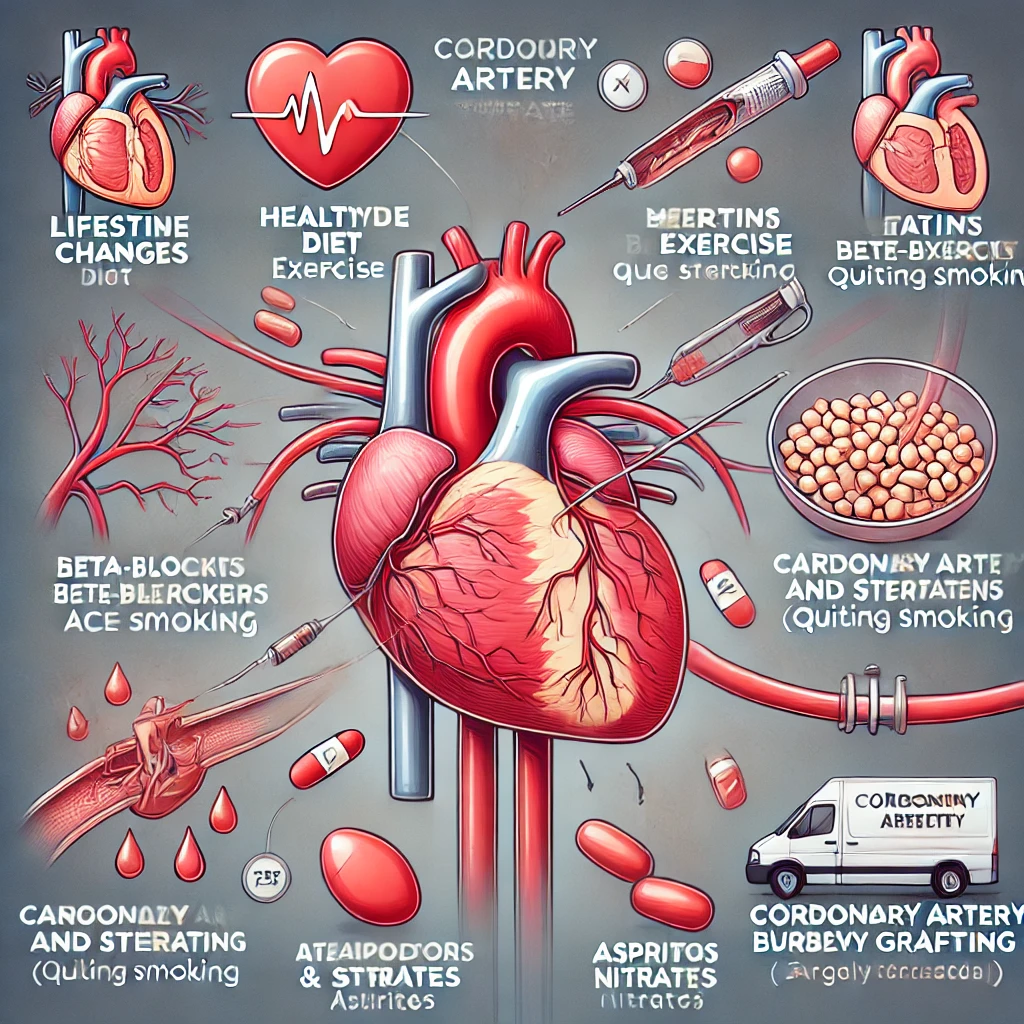
Lifestyle Changes
Adopting a healthy lifestyle is crucial in managing CAD and reducing the risk of complications. Key lifestyle changes include:
- Healthy Diet: Consuming a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help manage cholesterol levels and blood pressure.
- Regular Exercise: Engaging in at least 150 minutes of moderate-intensity exercise per week can improve heart health and reduce risk factors.
- Quitting Smoking: Smoking cessation is vital as it significantly reduces the risk of heart disease.
- Weight Management: Maintaining a healthy weight through diet and exercise can help control other risk factors such as diabetes and hypertension.
- Stress Management: Practicing stress-reducing techniques such as meditation, yoga, and deep breathing can improve overall heart health.
Medications
Medications are often prescribed to manage CAD and its risk factors. Common medications include:
- Statins: These drugs lower LDL cholesterol levels, reducing the risk of plaque buildup.
- **[Beta-Blockers](https://
en.wikipedia.org/wiki/Beta_blocker)**: They reduce heart rate and blood pressure, decreasing the heart’s demand for oxygen.
- ACE Inhibitors: These medications lower blood pressure and reduce strain on the heart.
- Aspirin: It helps to prevent blood clots, reducing the risk of heart attacks.
- Nitrates: These medications can relieve chest pain by dilating blood vessels.
Surgical and Procedural Interventions
In some cases, lifestyle changes and medications may not be sufficient to manage CAD. Surgical and procedural interventions may be necessary:
- Angioplasty and Stenting: A procedure that involves inserting a balloon-tipped catheter into the narrowed artery and inflating it to widen the artery. A stent (a small mesh tube) is then placed to keep the artery open.
- Coronary Artery Bypass Grafting (CABG): This surgery involves taking a blood vessel from another part of the body and using it to bypass the blocked coronary artery, restoring blood flow to the heart.
Rehabilitation and Follow-up
Cardiac rehabilitation programs are essential for patients recovering from a heart attack or surgery. These programs include supervised exercise, education on heart-healthy living, and counseling to help manage stress and improve quality of life.
Emerging Treatments
Advancements in medical research have led to the development of new and emerging treatments for CAD. Some of these include:
- Gene Therapy: Research is ongoing to explore the potential of gene therapy in treating CAD by promoting the growth of new blood vessels or improving the function of existing ones.
- Stem Cell Therapy: Studies are investigating the use of stem cells to repair damaged heart tissue and improve heart function in CAD patients.
- Immunotherapy: Emerging research is exploring the potential of immunotherapy in reducing inflammation and plaque buildup in the arteries.
Personalized Medicine
Personalized medicine involves tailoring treatment plans based on an individual’s genetic makeup, lifestyle, and other factors. This approach aims to optimize treatment outcomes and minimize side effects. Advances in genetic testing and molecular biology are paving the way for personalized medicine in the management of CAD.
Alternative and Complementary Therapies
In addition to conventional treatments, some patients may explore alternative and complementary therapies to manage CAD. These therapies should be used in conjunction with, not as a replacement for, standard medical treatments. Some alternative and complementary therapies include:
- Acupuncture: This traditional Chinese medicine practice involves inserting thin needles into specific points on the body to alleviate pain and improve overall health.
- Herbal Supplements: Certain herbal supplements, such as garlic, omega-3 fatty acids, and coenzyme Q10, may have beneficial effects on heart health.
- Mind-Body Techniques: Practices such as yoga, meditation, and tai chi can help reduce stress and improve overall well-being.
Monitoring and Follow-up Care
Ongoing monitoring and follow-up care are crucial for individuals with CAD. Regular check-ups with a healthcare provider can help track progress, adjust treatment plans, and manage any complications. Here are some key aspects of follow-up care:
- Regular Health Assessments: Routine assessments of blood pressure, cholesterol levels, and blood sugar can help monitor the effectiveness of treatment and make necessary adjustments.
- Symptom Monitoring: Patients should keep track of any new or worsening symptoms and report them to their healthcare provider promptly.
- Medication Adherence: Taking prescribed medications as directed is essential for managing CAD and preventing complications.
- Lifestyle Maintenance: Continuing with heart-healthy lifestyle changes, including diet, exercise, and stress management, is vital for long-term health.
Preventing Coronary Artery Disease
Healthy Lifestyle Choices
Preventing CAD involves making heart-healthy lifestyle choices. Here are some effective strategies:
- Balanced Diet: Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit saturated fats, trans fats, sodium, and added sugars.
- Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity exercise each week. Activities such as walking, cycling, and swimming can improve cardiovascular health.
- Smoking Cessation: Quitting smoking is one of the most significant steps you can take to improve heart health. Seek support through cessation programs or medications if needed.
- Weight Management: Achieving and maintaining a healthy weight can help control risk factors such as high blood pressure, diabetes, and high cholesterol.
- Stress Reduction: Incorporate stress management techniques into your daily routine. Practices such as mindfulness, meditation, and yoga can help reduce stress levels.
- Regular Health Screenings: Keep up with regular check-ups and screenings for blood pressure, cholesterol, and diabetes. Early detection and management of these conditions can prevent CAD.
Educational and Community Support
Community programs and educational initiatives can play a crucial role in preventing CAD. Participating in support groups, attending health seminars, and staying informed about heart health can motivate individuals to make positive lifestyle changes.
Role of Healthcare Providers
Healthcare providers play a vital role in CAD prevention. Regular consultations, personalized advice, and monitoring can help individuals manage risk factors effectively. It is essential to follow your healthcare provider’s recommendations and stay proactive about heart health.
Prevention Strategies for Specific Populations
Certain populations are at higher risk for CAD and may require targeted prevention strategies:
- Women: Women may experience different symptoms of CAD and have unique risk factors, such as hormonal changes during menopause. Tailored prevention strategies, including hormone replacement therapy (HRT) considerations and gender-specific education, can be beneficial.
- Elderly: Age is a significant risk factor for CAD. Elderly individuals should focus on maintaining a healthy lifestyle, managing comorbidities, and adhering to prescribed medications to reduce their risk.
- Diabetics: Diabetes significantly increases the risk of CAD. Managing blood sugar levels, following a heart-healthy diet, and regular monitoring are essential for preventing CAD in diabetic patients.
Impact of Socioeconomic Factors
Socioeconomic factors, including income, education, and access to healthcare, can influence the risk of CAD. Efforts to address these disparities through public health initiatives, policy changes, and community support programs can help reduce the burden of CAD in underserved populations.
Global Perspectives on Prevention
Different regions and cultures may have unique approaches to CAD prevention. Understanding and incorporating cultural practices, dietary habits, and traditional medicine can enhance prevention efforts globally. Collaborative efforts between healthcare providers, governments, and communities are essential for addressing the global burden of CAD.
Technological Advancements in Prevention
Advancements in technology have the potential to revolutionize CAD prevention:
- Wearable Devices: Wearable devices, such as fitness trackers and smartwatches, can monitor physical activity, heart rate, and other health metrics, providing valuable data for preventive measures.
- Mobile Health Apps: Mobile applications can offer personalized health recommendations, track progress, and provide reminders for medication and appointments.
- Telemedicine: Telemedicine allows for remote consultations, making it easier for individuals to access healthcare services and receive preventive care.
Preventive Medications
In some cases, medications may be prescribed to reduce the risk of CAD. These medications include:
- Statins: These drugs lower LDL cholesterol levels, reducing the risk of plaque buildup.
- Aspirin: Low-dose aspirin may be prescribed to prevent blood clots in high-risk individuals.
- Blood Pressure Medications: Medications such as beta-blockers, ACE inhibitors, and diuretics can help control blood pressure and reduce the risk of CAD.
Preventive Health Programs
Public health programs aimed at promoting heart health and preventing CAD are essential. These programs may include:
- Community Health Education: Workshops, seminars, and educational campaigns to raise awareness about CAD and promote healthy lifestyle choices.
- Screening Programs: Regular screenings for blood pressure, cholesterol, and diabetes can help detect risk factors early.
- Fitness Initiatives: Community-based fitness programs and facilities to encourage physical activity.
Living with Coronary Artery Disease
Managing Symptoms
Living with CAD requires ongoing management of symptoms and adherence to treatment plans. Here are some tips for managing symptoms:
- Monitor Symptoms: Keep track of any changes in symptoms and report them to your healthcare provider.
- Follow Medication Regimen: Take prescribed medications as directed and do not skip doses.
- Lifestyle Modifications: Continue with heart-healthy lifestyle changes, including diet, exercise, and smoking cessation.
- Manage Stress: Incorporate stress-reducing activities into your daily routine to help manage symptoms and improve overall well-being.
Emotional and Psychological Aspects
Living with CAD can be emotionally challenging. It is common to experience feelings of anxiety, depression, or fear. Here are some ways to address these emotional aspects:
- Seek Support: Join support groups or counseling sessions to connect with others facing similar challenges.
- Communicate with Loved Ones: Share your feelings and concerns with family and friends to build a strong support system.
- Practice Mindfulness: Engage in mindfulness practices such as meditation or deep breathing exercises to reduce stress and improve mental well-being.
Having access to support networks and resources can make living with CAD more manageable. Here are some valuable resources:
- Cardiac Rehabilitation Programs: Participate in cardiac rehab programs to receive supervised exercise, education, and support.
- Patient Education Materials: Utilize educational materials provided by healthcare organizations to stay informed about CAD and its management.
- Online Communities: Join online forums and communities to connect with others living with CAD and share experiences.
Long-term Management
Long-term management of CAD involves regular monitoring, adherence to treatment plans, and lifestyle modifications. Here are some key aspects of long-term management:
- Regular Check-ups: Schedule regular check-ups with your healthcare provider to monitor your condition and adjust treatment plans as needed.
- Medication Adherence: Take medications as prescribed and discuss any side effects or concerns with your healthcare provider.
- Healthy Lifestyle: Maintain a heart-healthy lifestyle, including a balanced diet, regular exercise, and stress management.
- Monitoring Symptoms: Keep track of any changes in symptoms and report them promptly to your healthcare provider.
Emergency Preparedness
Being prepared for emergencies is essential for individuals with CAD. Here are some tips for emergency preparedness:
- Know the Signs of a Heart Attack: Be aware of the signs and symptoms of a heart attack and seek immediate medical attention if they occur.
- Keep Emergency Contacts Handy: Have a list of emergency contacts, including your healthcare provider and local emergency services, readily available.
- Carry Medical Information: Carry a card or bracelet with information about your medical condition, medications, and any allergies.
Advocating for Yourself
As a patient with CAD, advocating for yourself and being proactive about your health is crucial. Here are some ways to advocate for yourself:
- Ask Questions: Don’t hesitate to ask your healthcare provider questions about your condition, treatment options, and any concerns you may have.
- Stay Informed: Educate yourself about CAD and stay updated on the latest research and treatment options.
- Participate in Your Care: Be an active participant in your care by following treatment plans, attending appointments, and making informed decisions about your health.
Quality of Life
Maintaining a good quality of life is important for individuals with CAD. Here are some tips to improve your quality of life:
- Stay Active: Engage in regular physical activity that is safe and appropriate for your condition.
- Eat Well: Follow a heart-healthy diet that provides the necessary nutrients and supports overall health.
- Stay Connected: Maintain social connections and participate in activities that bring you joy and fulfillment.
- Manage Stress: Incorporate stress-reducing activities into your daily routine to improve mental well-being.
Conclusion
Coronary Artery Disease (CAD) is a serious condition that requires awareness, early detection, and effective management. By understanding the causes, recognizing the symptoms, and following appropriate treatment plans, individuals can lead healthier lives despite having CAD. Adopting heart-healthy lifestyle changes and seeking regular medical care are essential steps in preventing and managing this condition. Stay informed, stay proactive, and prioritize your heart health.
References
- World Health Organization (WHO)
- Centers for Disease Control and Prevention (CDC)
- American Heart Association
- National Heart, Lung, and Blood Institute (NHLBI)
- Mayo Clinic
- Johns Hopkins Medicine
- Cleveland Clinic
- Harvard Health Publishing
- British Heart Foundation
- European Society of Cardiology
Read also




