What is Dengue Shock Syndrome?
Dengue Shock Syndrome (DSS) is a severe, life-threatening complication of dengue fever, a tropical illness transmitted to humans through the bite of an infected Aedes mosquito. While sounding quite alarming, this disease is rare compared to the usual dengue fever. Yet, when it does occur, it can lead to serious health consequences if not promptly addressed.
The term “shock” in DSS refers to a medical condition where the blood pressure drops to dangerously low levels, restricting the amount of blood and oxygen reaching the body’s organs. This sudden drop in blood pressure is the defining symptom of DSS, hence its name.
The Cause: Dengue Fever
Have you ever been bitten by a mosquito? The type that carries the dengue virus is called Aedes aegypti. When these infected mosquitoes bite humans, the virus enters our bloodstream and may lead to dengue fever.
From Dengue Fever to Dengue Shock Syndrome: An In-depth Look
Dengue fever is an infectious disease transmitted through the bite of an infected Aedes mosquito. While most people with dengue fever recover within a week or two, a small percentage develop a severe and life-threatening form known as Dengue Shock Syndrome (DSS). Understanding how dengue fever progresses to DSS is critical, especially for those living in dengue-prone areas. But before we dive deep into the progression, let’s understand the basics of dengue fever.
Dengue Fever: The Beginning
The journey begins with a simple mosquito bite. The Aedes mosquito, mainly the Aedes aegypti and Aedes albopictus species, are carriers of the dengue virus. When this mosquito bites a person, the virus enters the bloodstream and starts to multiply.
The first signs of dengue fever usually appear 4 to 7 days after the infected mosquito bite. These may include high fever, severe headaches, pain behind the eyes, joint and muscle pain, and a skin rash that looks like measles. Most people recover within a week with adequate rest and hydration.
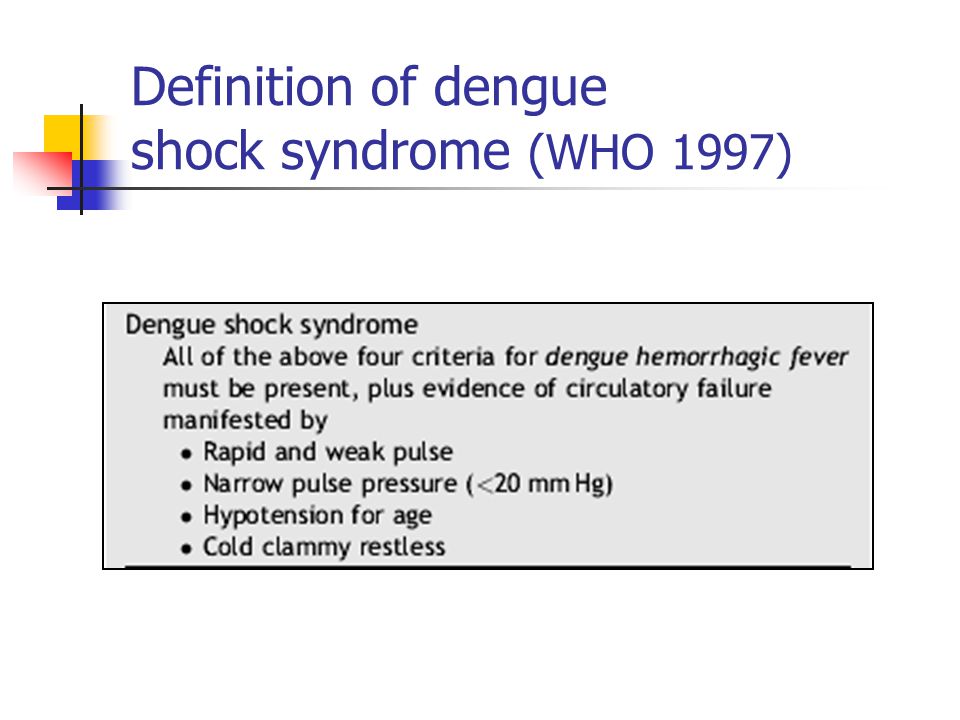
The Turn for the Worse: Dengue Hemorrhagic Fever and Dengue Shock Syndrome
However, dengue fever can take a more dangerous turn for some, progressing to Dengue Hemorrhagic Fever (DHF) or Dengue Shock Syndrome. It’s crucial to note that not everyone who gets dengue fever will develop DHF or DSS. The exact reason why some people progress to DHF or DSS is not fully understood, but certain factors appear to increase the risk.
One critical risk factor is having antibodies to the dengue virus from a previous infection. There are four types of dengue viruses (DENV-1, DENV-2, DENV-3, DENV-4). Getting infected with one type provides immunity to that type but only temporary immunity to the others. If a person is infected with a different type again, the risk of developing severe dengue, including DHF and DSS, is significantly increased.
This enhanced risk is thought to be due to antibody-dependent enhancement (ADE). Here, instead of protecting the person, the antibodies from the first infection help the new type of dengue virus to enter cells more efficiently, leading to a more severe infection.
The immune response also plays a role in the progression of the disease. In severe dengue cases, the immune system’s response is unusually high and uncontrolled, causing damage to the body’s cells.
Signs and Symptoms of Dengue Shock Syndrome
Early Warning Signs
As we know, Dengue Shock Syndrome (DSS) is a severe manifestation of dengue fever. The early detection of this condition is critical in preventing complications and improving patient outcomes. Therefore, it’s essential to understand the early warning signs associated with DSS. Here, we’ll dive deep into these warning signs, providing an understanding of what to look out for.
The Onset of Dengue Fever: The Initial Signs
The progression to Dengue Shock Syndrome begins with the onset of dengue fever. Typically, the signs and symptoms of dengue fever appear 4 to 7 days after being bitten by an infected Aedes mosquito. The initial symptoms are often flu-like and may include:
- High fever: This is usually the first sign, where the body temperature rises to 104 F degrees or higher.
- Severe headache and eye pain: Patients often describe a severe headache and pain behind the eyes, especially when moving them.
- Muscle, bone, and joint pain: Dengue fever is also known as “breakbone fever” because it can cause severe muscle, bone, and joint pain.
- Rash: Many people develop a rash that can spread from the torso to the arms, legs, and face. The rash is typically itchy and may appear a few days after the fever starts.
- Nausea and vomiting: Patients may experience a loss of appetite, nausea, and vomiting.
Transitioning to Dengue Shock Syndrome: The Warning Signs
Additional warning signs typically appear if dengue fever progresses to Dengue Shock Syndrome. These signs usually manifest when the fever begins to subside, 3-7 days after the onset of symptoms. Key warning signs include:
- Severe abdominal pain: A sudden, persistent and severe pain in the abdomen is a common early warning sign of DSS.
- Persistent vomiting: While vomiting can be a symptom of dengue fever, persistent vomiting is a critical warning sign that the disease may progress to DSS.
- Rapid breathing: As the body tries to compensate for the lack of oxygen due to reduced blood flow, the person may start to breathe rapidly.
- Bleeding: Spontaneous bleeding can occur from the nose, gums, or under the skin. You may also notice blood in vomit, urine, or stool.
- Fatigue and restlessness: As DSS progresses, you may feel unusually tired, restless, or lethargic.
- Cold, clammy skin: Reduced blood circulation can make the skin feel cold and clammy.
- The rapid drop in blood pressure: One of the defining symptoms of DSS is a sudden drop in blood pressure, which may make the person feel faint or lightheaded.
- Weak, rapid pulse: As the body goes into shock, the pulse may become weak, fast, and difficult to feel or measure.
- Decreased urination: A significant decrease in urination could indicate shock and should be considered an emergency.
If these warning signs are noticed, immediate medical attention is needed. Dengue Shock Syndrome can progress rapidly and lead to life-threatening complications, including organ damage, heart problems, and death.
Remember, early detection and access to proper medical care lowers the risk of complications and can significantly increase the chances of a full recovery. Therefore, seek immediate medical assistance if you or a loved one has dengue fever and begins to show any of these warning signs.
The fight against Dengue Shock Syndrome begins with awareness. Recognizing the early warning signs empowers us to act swiftly and seek prompt medical intervention. Our knowledge is our most robust defence against this potentially severe and life-threatening condition.
Who is at Risk for Dengue Shock Syndrome?
Regarding Dengue Shock Syndrome (DSS), specific populations are at a higher risk than others. Understanding these risk factors can help in the early detection, prompt treatment, and effective prevention of the disease. Let’s delve into the groups most susceptible to DSS.
1. Geographic Location
One of DSS’s most significant risk factors is living in or travelling to a tropical or subtropical region. Dengue fever and, by extension, DSS are endemic in more than 100 countries worldwide, including parts of Southeast Asia, the Western Pacific islands, Latin America, and Africa. Outbreaks also occur occasionally in the Caribbean and along the southeastern seaboard of the United States.
2. Prior Dengue Infection
A person infected with the dengue virus is at an increased risk of developing severe dengue, including DSS, during a subsequent infection. This is because there are four different serotypes of the dengue virus. Once infected with one serotype, they develop lifelong immunity against that particular serotype but only temporary immunity against the others. If infected with a different serotype later, the disease can be much more severe—a phenomenon known as antibody-dependent enhancement (ADE).
3. Age and Health Status
While anyone can get dengue fever, younger children and those with weaker immune systems are at a higher risk of developing DSS. Certain pre-existing health conditions, like diabetes and heart disease, can also increase the risk of severe dengue complications.
4. Genetic Factors
Certain genetic factors might make some individuals more susceptible to severe dengue. Studies suggest that people of certain ethnicities, such as African or Caucasian descent, may have a lower risk of severe dengue than others.
In conclusion, while DSS can affect anyone, individuals living in or travelling to endemic areas, those with previous dengue infection, young children, individuals with compromised immunity, and certain genetic factors put individuals at a higher risk. Awareness of these risk factors can guide targeted preventive measures, aiding in the fight against this potentially fatal condition.
Diagnosis of Dengue Shock Syndrome: A Detailed Guide
Dengue Shock Syndrome (DSS) is a severe form of dengue fever, a disease transmitted by the Aedes mosquito. Due to its potential to lead to life-threatening complications, early diagnosis of DSS is critical. In this guide, we will delve deep into the process of diagnosing DSS, looking at everything from initial symptoms to the lab tests used for confirmation.
The Journey to Diagnosis: Initial Symptoms
The journey to diagnosing Dengue Shock Syndrome starts with the recognition of symptoms. As discussed in earlier sections, initial symptoms of dengue fever resemble those of a flu-like illness, which typically manifest 4 to 7 days after a bite from an infected mosquito. The progression to DSS is usually marked by new and severe symptoms such as severe abdominal pain, persistent vomiting, rapid breathing, bleeding, and signs of shock like cold and clammy skin, weak pulse, and restlessness.
If a patient presents with these symptoms, especially in a dengue-prone area or has recently travelled to one, the healthcare provider would likely suspect dengue fever and its severe forms like DSS.
Clinical Examination and Medical History
The healthcare provider will conduct a physical examination, focusing on the vital signs (temperature, heart rate, respiratory rate, and blood pressure), signs of bleeding, rash, and other symptoms associated with dengue fever and DSS.
Additionally, a detailed medical history is essential. The healthcare provider will ask questions about the onset of symptoms, recent travels, prior dengue infections, and other health conditions. The patient’s exposure to mosquito-infested areas will also be explored.
Laboratory Testing: The Key to Confirmation
The suspicion of Dengue Shock Syndrome is confirmed through laboratory testing. These tests not only verify the presence of the dengue virus but also provide crucial information on the severity of the disease. The primary diagnostic tests include:
- Dengue virus tests: These tests directly detect the presence of the virus or its components. They include the dengue virus detection test, which identifies the virus in the blood within the first week of illness, and the dengue virus antigen detection tests, which detect proteins (non-structural protein one or NS1) produced by the dengue virus.
- Antibody tests: These tests look for antibodies against the dengue virus in the blood. The antibodies are proteins produced by the immune system in response to the infection. There are two types of antibodies: IgM and IgG. IgM antibodies are produced first and can usually be detected in the blood within a few days after the onset of symptoms. IgG antibodies appear later and can remain in the bloodstream for several months or even years.
- Blood tests: These tests are essential to determine the severity of the disease. They include a complete blood count (CBC), which examines different types of cells in the blood. The healthcare provider will look for a low platelet count (thrombocytopenia), which can indicate bleeding complications, and a high or low white blood cell count, which reflects the body’s immune response to the infection. The hematocrit level is also monitored; a high one can indicate dehydration, while a sudden drop may suggest bleeding.
- Biochemical tests: These tests assess the functioning of the liver and heart by measuring enzymes and other substances in the blood. Elevated levels of liver enzymes (AST and ALT) may indicate liver damage, a common complication of severe dengue. Electrolyte levels, creatinine, and other biochemical parameters may also be evaluated to assess kidney function and the overall metabolic state of the body.
Imaging Tests
Although not routinely used to diagnose DSS, imaging tests such as ultrasound or CT scans may be used in some instances to check for fluid accumulation in body cavities, which is a sign of severe dengue.
In conclusion, the diagnosis of Dengue Shock Syndrome is a multifaceted process that involves symptom recognition, clinical examination, detailed medical history, and a range of laboratory tests. Understanding this process can help ensure timely diagnosis and treatment, minimizing the risk of severe complications. As we’ve said before, early recognition and prompt medical attention are our most potent weapons against DSS, and knowing the journey to diagnosis is an integral part of this battle.
Treatment Options for Dengue Shock Syndrome
Dengue Shock Syndrome (DSS) is a severe dengue fever manifestation requiring immediate medical attention. There is no specific antiviral medication for treating DSS; management is typically supportive, focusing on relieving symptoms and preventing complications. In this guide, we will explore the various treatment options for DSS, taking a closer look at each stage of medical intervention.
Emergency Medical Intervention
DSS is a medical emergency. Immediate treatment is required to prevent shock, organ damage, or death. The treatment strategy typically focuses on replacing lost fluids and maintaining vital organ functions.
- Fluid Replacement: Intravenous (IV) fluid replacement is critical in managing DSS. The goal is to replace lost fluids and electrolytes and maintain adequate blood volume and blood pressure. This treatment can prevent the patient from going into shock.
- Oxygen Therapy: Oxygen may be administered to ensure adequate oxygen supply to the organs, especially if the patient shows signs of respiratory distress.
- Monitoring Vital Signs: Regular monitoring of blood pressure, heart rate, respiratory rate, and temperature is vital to assess the patient’s condition and adjust treatment as needed.
Hospitalization and Ongoing Care
Patients with DSS often need to be hospitalized for close monitoring and treatment. Hospital care usually involves:
- Continued Fluid Management: Doctors will closely monitor the patient’s hydration status, adjusting fluid volumes and rates as necessary.
- Blood Transfusion: A blood transfusion may be required if severe bleeding occurs or the patient’s platelet count drops significantly.
- Electrolyte Correction: Electrolytes, essential for many body functions, may become imbalanced during the disease. If necessary, they will be corrected using medications or IV fluids.
- Pain Management: Medications may be given to alleviate pain and reduce fever. However, aspirin and non-steroidal anti-inflammatory drugs (NSAIDs) are typically avoided because they can increase the risk of bleeding.
- Regular Lab Tests: Frequent blood tests are performed to monitor the disease progression, assess organ function, and guide treatment decisions.
Post-Hospital Care and Rehabilitation
Once the critical phase has passed, the patient will continue to be monitored as they recover. This often involves:
- Gradual Fluid Withdrawal: As the patient’s condition stabilizes, IV fluids are gradually withdrawn. Oral rehydration is encouraged.
- Nutritional Support: Proper nutrition is crucial for recovery. The patient may receive dietary advice or nutritional supplements.
- Physical Rehabilitation: If DSS has led to any physical weakness or complications, physical therapy might be needed as part of the recovery process.
Prevention: The Best Treatment
The best treatment for DSS is prevention. This involves avoiding mosquito bites (using insect repellent, wearing long sleeves and pants, using bed nets, etc.) and implementing public health measures to control the mosquito population. Vaccines against the dengue virus are also available in some countries and can be administered to individuals living in endemic areas.
In conclusion, managing Dengue Shock Syndrome is a complex process requiring immediate emergency interventions, hospitalization, ongoing care, and post-hospital rehabilitation. Although there’s currently no specific antiviral treatment for DSS, prompt supportive care can significantly improve outcomes and reduce mortality. And remember, prevention is always the best strategy in the battle against dengue.
Preventing Dengue Shock Syndrome
Mosquito Control
Reducing exposure to mosquitoes is crucial. Use repellents, wear protective clothing, and eliminate standing water near your home.
Vaccines and Medications
A dengue vaccine is available in some countries but is not yet universally recommended due to limited efficacy.
Dengue Shock Syndrome: A Global Health Concern
DSS is not just a personal health risk but a global one. It affects millions every year, especially in tropical regions. Awareness and prevention are crucial to combat this threat.
Conclusion
Understanding DSS is the first step towards prevention. Remember, it’s not just about protecting yourself but also helping to reduce the global impact of this disease.
FAQs about Dengue Shock Syndrome
- What is Dengue Shock Syndrome?
Dengue Shock Syndrome (DSS) is a severe form of dengue fever characterized by a rapid drop in blood pressure, leading to symptoms of shock. - What causes Dengue Shock Syndrome?
DSS is caused by an infection with the dengue virus, usually due to a secondary infection with a different serotype than the initial infection. The body’s immune response to the virus typically leads to severe symptoms of DSS. - What are the symptoms of Dengue Shock Syndrome?
Symptoms of DSS may include sudden onset of high fever, severe abdominal pain, vomiting, rapid breathing, and signs of shock like cold, clammy skin, restlessness, and weak, rapid pulse. - How is Dengue Shock Syndrome diagnosed?
DSS is diagnosed based on clinical symptoms, medical history, and various lab tests, including blood tests to detect the virus or antibodies against it and tests to assess organ function, platelet count, and hematocrit levels. - How is Dengue Shock Syndrome treated?
Treatment for DSS is mainly supportive and focuses on maintaining fluid balance, treating symptoms, and preventing complications. This often involves intravenous fluid therapy, close monitoring of vital signs, and sometimes a blood transfusion. - Can Dengue Shock Syndrome be prevented?
Prevention strategies mainly involve avoiding mosquito bites and controlling mosquito populations. Vaccines against dengue are available in some countries and can provide some protection. - Who is at risk for Dengue Shock Syndrome?
Anyone can get DSS if infected with the dengue virus. Still, the risk is higher in individuals who have a secondary infection with a different dengue serotype than their initial infection. - What is the prognosis for Dengue Shock Syndrome?
With prompt and adequate treatment, most people recover from DSS. However, it can be fatal if not treated promptly. - What is the difference between Dengue Fever and Dengue Shock Syndrome?
While the dengue virus causes both, DSS is a more severe form that includes symptoms of shock. Dengue fever generally has milder symptoms like fever, headache, and joint and muscle pain. - What complications can arise from Dengue Shock Syndrome?
Complications can include severe bleeding, organ damage due to reduced blood flow, and metabolic disturbances. - Can you get Dengue Shock Syndrome more than once?
While a previous infection with one dengue virus serotype can provide lifelong immunity against that serotype, it doesn’t prevent infection with the other serotypes. Subsequent infection with a different serotype can lead to severe dengue, including DSS. - Why does a second infection with dengue often lead to more severe disease?
This is mainly due to antibody-dependent enhancement (ADE), where antibodies from the first infection help the virus from a different serotype enter cells during a second infection, leading to an increased viral load. - How long after dengue fever can Dengue Shock Syndrome occur?
DSS usually develops after 3-7 days of dengue fever, often when the fever starts to subside. - What is plasma leakage in Dengue Shock Syndrome?
Plasma leakage is a condition where plasma, the fluid part of blood, leaks out of the blood vessels into surrounding tissues. This can lead to a drop in blood volume and blood pressure, resulting in shock. - Why does plasma leakage occur in Dengue Shock Syndrome?
Plasma leakage is thought to be due to the effects of cytokines and other immune response factors on the blood vessels, making them more permeable or ‘leaky’. - Can Dengue Shock Syndrome lead to organ failure?
Yes, in severe cases, the drop in blood pressure can reduce blood flow to vital organs, leading to organ failure. - How quickly do you need to treat Dengue Shock Syndrome?
DSS is a medical emergency and requires immediate treatment to prevent shock, organ damage, or even death. - What role do platelets play in Dengue Shock Syndrome?
Platelets help in blood clotting. In dengue, the platelet count can drop significantly (a condition called thrombocytopenia), increasing the risk of bleeding. - Is Dengue Shock Syndrome contagious?
No, DSS itself is not contagious. The dengue virus, which causes DSS, is transmitted through the bite of an infected Aedes mosquito, not from person to person. - What research is being done on Dengue Shock Syndrome?
Research is ongoing to understand DSS pathophysiology better, improve diagnostic tests, develop specific antiviral treatments, and create more effective vaccines.
References
- World Health Organization: Dengue and severe dengue
- CDC: Dengue
- Mayo Clinic: Dengue Fever
- National Institute of Allergy and Infectious Diseases: Dengue Fever
- MedlinePlus: Dengue
My other articles:
- What Triggers Fever: An In-depth Look into the Heat of the Matter
- Dengue Fever: Symptoms, Causes, Diagnosis, Treatment, and Prevention
- Understanding Dengue Hemorrhagic Fever: Causes, Symptoms, and Prevention
- The Pattern of Fever: A Comprehensive Overview
- Unravelling the Mysteries of Myocardial Infarction: A Comprehensive Guide
Disclaimer This article is intended for informational purposes only and does not constitute medical advice. The information herein is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read in this article.




