Introduction
Brief overview of the gallbladder and its function
The Gallbladder: Structure, Location, and Function
- The human body is a marvel of engineering and design, with each organ playing a unique role in maintaining optimal health. One such organ, often underestimated in its significance but essential in function, is the gallbladder.
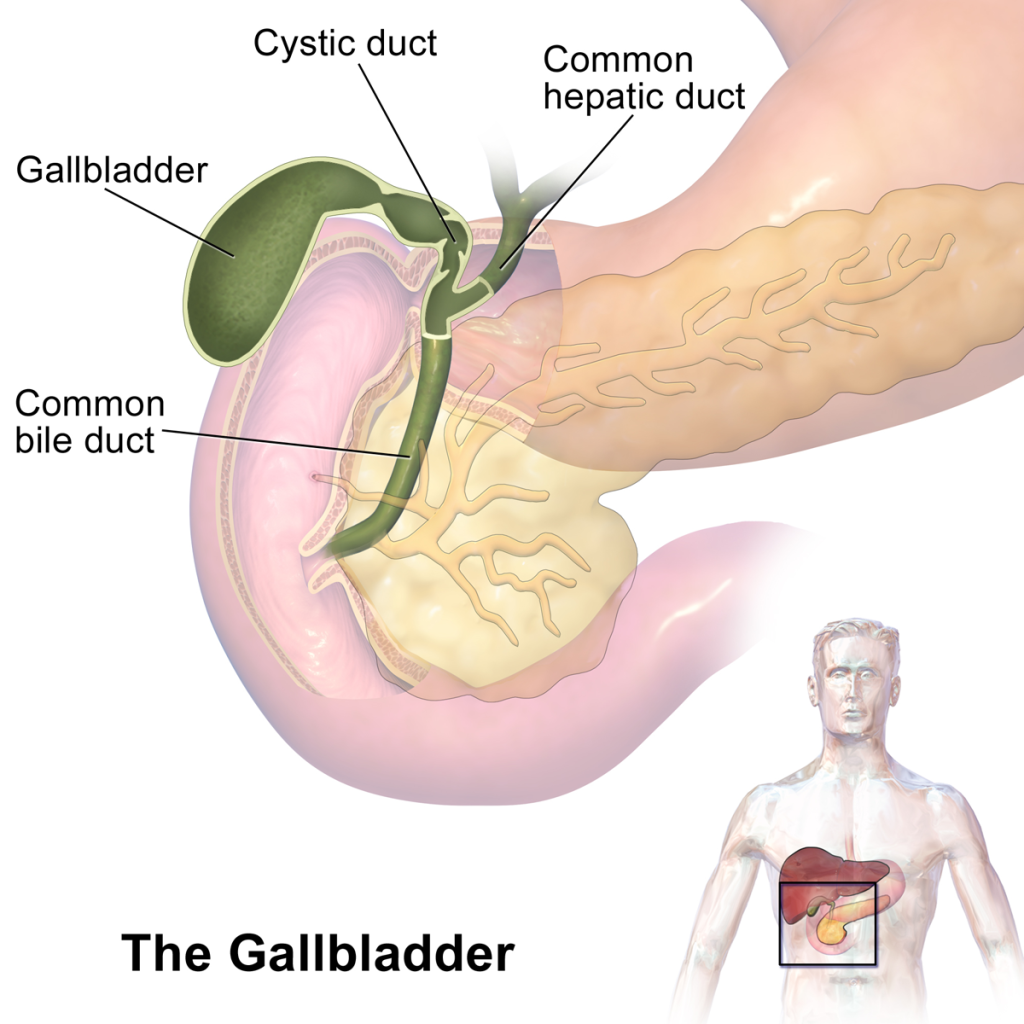
- Location and Physical Description: The gallbladder is a small, pear-shaped organ nestled just beneath the liver on the right side of the abdomen. Despite its small size, typically about 8 cm in length and holding approximately 30 to 50 ml of fluid when full, the gallbladder plays a pivotal role in the digestive process.
- Structure: The gallbladder’s wall comprises three layers: an inner lining (mucosa), a muscular layer, and an outer layer (serosa). The mucosa forms several small folds known as rugae, which allow the gallbladder to expand and contract. The cystic duct connects the gallbladder to the common bile duct, which subsequently opens into the small intestine.
- Function – Bile Storage and Concentration: One of the primary functions of the gallbladder is to store and concentrate bile. Bile is a greenish-brown alkaline fluid produced by hepatocytes in the liver. Composed of water, cholesterol, fats, bile salts, proteins, and bilirubin, bile plays a crucial role in the digestion and absorption of fats and fat-soluble vitamins (like vitamins A, D, E, and K).
- After production in the liver, bile flows into the bile ducts. When not immediately required for digestion, bile is directed into the gallbladder for storage. Here, the gallbladder reabsorbs water and some electrolytes from the bile, increasing its concentration and making it up to ten times more potent than the bile produced by the liver.
- Function – Bile Release and Fat Digestion: When we consume food, particularly fatty foods, the presence of chyme (partially digested food) in the small intestine triggers the release of a hormone called cholecystokinin (CCK). CCK signals the gallbladder to contract, thereby releasing the stored, concentrated bile into the small intestine via the common bile duct. Once in the small intestine, bile aids in the emulsification of fats, breaking them down into smaller droplets. This process increases the surface area of fats, making them more accessible to digestive enzymes, and facilitating their absorption into the bloodstream.
- While the gallbladder might seem like a mere storage unit, it’s evident that its role in the digestive process is indispensable. By storing and concentrating bile, the gallbladder ensures that our body has a readily available supply of this essential fluid to efficiently digest fats whenever we consume them. The intricate interplay between the gallbladder, liver, and small intestine showcases the body’s exceptional ability to coordinate various organs towards a singular goal: optimal digestion. However, it’s worth noting that while the gallbladder significantly aids in fat digestion, humans can survive without it. If removed due to medical conditions, the liver continues to produce bile, but it drips continuously into the small intestine rather than being stored and concentrated. This setup underscores the body’s remarkable adaptability and resilience.
Reasons for gallbladder removal
The removal of the gallbladder, known medically as a cholecystectomy, is a common procedure. There are several reasons why a gallbladder might need to be removed, including:
- Gallstones (Cholelithiasis): These are hard particles that develop in the gallbladder and can block the normal flow of bile. They can cause pain, nausea, vomiting, and other digestive symptoms.
- Gallbladder Inflammation (Cholecystitis): This is the inflammation of the gallbladder, often caused by a blocked duct or gallstones. Symptoms can include severe pain, fever, and tenderness in the upper right abdomen.
- Biliary Dyskinesia: This is a condition where the gallbladder doesn’t empty bile correctly due to a defect in the gallbladder’s motility. Symptoms can be similar to those of gallstones.
- Gallbladder Polyps: These are growths that arise from the lining of the gallbladder. While most are benign, some larger polyps can harbor or evolve into malignancies.
- Gallbladder Cancer: While rare, cancer of the gallbladder requires its removal to prevent the spread of the disease.
- Pancreatitis: This is inflammation of the pancreas, and it can be due to gallstones blocking the pancreatic duct.
- Gallstone Ileus: A rare complication where a large gallstone migrates into the intestine and causes a blockage.
- Porcelain Gallbladder: This is a condition where the walls of the gallbladder become calcified. It is associated with an increased risk of gallbladder cancer.
- Other Complications: Sometimes, complications from other surgeries or procedures (like ERCP) can injure the gallbladder or its ducts, necessitating its removal.
Types of gallbladder surgeries
The gallbladder, a small organ tasked with storing and concentrating bile, can sometimes become a source of significant discomfort and illness. A variety of diseases can afflict this organ, most commonly gallstones, which may necessitate surgical intervention. Gallbladder surgery, commonly referred to as cholecystectomy, has evolved over the years, leading to the development of multiple techniques tailored to individual needs and specific conditions. Let’s delve deep into the various types of gallbladder surgeries.
1. Open Cholecystectomy:
Description: This is a traditional surgical method wherein a large incision is made in the abdomen to access and remove the gallbladder.
Procedure: After anesthesia is administered, a 5-7 inch incision is typically made just below the ribs on the right side. The surgeon will then identify the gallbladder, separate it from its attachments, and remove it.
Recovery: The healing time for open cholecystectomy is relatively long, usually ranging from 6 to 8 weeks. Due to the larger incision, there might be more post-operative pain and a more noticeable scar.
2. Laparoscopic Cholecystectomy:
Description: Often referred to as ‘keyhole surgery’, this technique utilizes small incisions and a laparoscope (a thin tube with a camera) to remove the gallbladder.
Procedure: Around 3 to 4 tiny incisions are made in the abdomen. The laparoscope, along with specialized instruments, is inserted. The surgeon views the operation on a video screen, carefully detaching the gallbladder before extracting it through one of the incisions.
Recovery: This method boasts a shorter recovery time, generally within a week. There’s less post-operative pain, and scars are minimal.
3. Single Incision Laparoscopic Surgery (SILS):
Description: A more recent innovation, SILS is a form of laparoscopic surgery conducted via a single incision, typically made in the navel.
Procedure: Specialized instruments and a laparoscope are inserted through a solitary incision in the navel. The gallbladder is then detached and removed through this single point.
Recovery: SILS generally offers a quicker recovery and virtually scarless outcome, as the incision is hidden within the navel.
4. Robot-Assisted Cholecystectomy:
Description: In this approach, surgeons utilize robotic technology to aid in the gallbladder’s removal.
Procedure: After making a few small incisions, the surgeon uses a console to control robotic arms, which provide precision, flexibility, and control beyond conventional techniques.
Recovery: Recovery is comparable to the laparoscopic approach, with patients often resuming normal activities within a week.
5. Percutaneous Cholecystostomy:
Description: Rather than a standard gallbladder removal, this procedure involves placing a tube into the gallbladder to drain its contents. It’s often used for patients who are too ill for surgery.
Procedure: Under imaging guidance, a catheter is inserted through the skin and directly into the gallbladder. Bile and any gallstones are then drained out.
Recovery: Since it’s a less invasive procedure, recovery can be faster. However, this is typically a temporary solution until the patient is well enough for a cholecystectomy.
6. Natural Orifice Transluminal Endoscopic Surgery (NOTES):
Description: This is an experimental procedure where instruments are inserted through a natural orifice, like the mouth or vagina, eliminating the need for external incisions.
Procedure: The surgeon accesses the gallbladder through an orifice, uses endoscopic tools to detach it, and then removes it through the same orifice.
Recovery: Since there are no external incisions, scarring is nonexistent, and recovery might be quicker.
7. Partial Cholecystectomy:
Description: As the name suggests, this procedure involves removing only a part of the gallbladder, usually when a complete removal might be too risky.
Procedure: This is generally done when the gallbladder is too inflamed or has adhered too closely to surrounding structures, making full removal dangerous. Only the portion of the gallbladder that can be safely accessed is removed.
Recovery: Recovery time varies but is generally similar to that of an open cholecystectomy.
The decision regarding which type of gallbladder surgery to undergo often depends on the specific diagnosis, the patient’s health, the surgeon’s expertise, and the available facilities. While laparoscopic cholecystectomy remains the most common procedure, the advent of new technologies and techniques ensures that patients have multiple options tailored to their unique needs. As with all surgeries, it’s vital to understand the benefits, risks, and recovery expectations associated with each type of cholecystectomy. Discussing these aspects with a healthcare professional can provide clarity and ensure that patients make informed decisions about their health.

Pre-operative preparations
Preparing for gallbladder surgery, or cholecystectomy, is crucial to ensure a smooth surgical procedure and recovery. Here’s a comprehensive guide to the steps and precautions patients typically need to take prior to the surgery:
1. Medical Evaluation:
- Physical Examination: A thorough check-up will be done to assess the patient’s overall health and to ensure they’re fit for surgery.
- Blood Tests: These help determine liver function, blood clotting, and other vital parameters.
- Imaging Studies: Ultrasound or other imaging tests might be reviewed or conducted to get a clear picture of the gallbladder’s condition.
2. Medications:
- Review Current Medications: Patients should provide a list of all medications they’re currently taking, including over-the-counter drugs, vitamins, and supplements.
- Adjust Medications: Some medications, especially blood thinners or non-steroidal anti-inflammatory drugs (NSAIDs), may need to be stopped or adjusted prior to the surgery.
- Avoid Herbal Supplements: Some herbal products can increase bleeding risk, so it’s essential to discuss any natural remedies or supplements with the doctor.
3. Fasting:
- Typically, patients are instructed not to eat or drink anything for 6 to 12 hours before the surgery, especially if general anesthesia will be used. This precaution helps prevent aspiration during the procedure.
4. Bowel Preparation:
- In some cases, doctors might recommend a bowel prep solution or laxatives to clear out the intestines. This is not as common for gallbladder surgery as it is for other procedures, but it’s essential to follow any guidelines provided.
5. Hygiene:
- Patients might be asked to bathe or shower with a special antiseptic soap the night before or the morning of the surgery to reduce the risk of infection.
6. Arrange for Post-Operative Care:
- Ensure someone is available to drive the patient home post-surgery, especially if it’s an outpatient procedure.
- It might also be helpful to have someone stay with the patient for the first 24 hours after the surgery to assist with basic tasks.
7. What to Bring to the Hospital:
- Carry all essential paperwork, including insurance details and identification.
- Bring a list of medications and known allergies.
- Carry personal items like glasses, hearing aids, dentures, etc. However, these will need to be removed before the surgery.
8. What to Avoid:
- Do not wear jewelry, nail polish, or makeup on the day of the surgery.
- Avoid using lotions or creams.
9. Stay Informed:
- Make sure to understand the procedure fully. Don’t hesitate to ask the doctor or surgical team any questions about the surgery, risks, benefits, and recovery process.
- Ensure informed consent forms are signed after understanding all implications.
10. Mind and Body Preparation:
- Engaging in relaxation techniques, like deep breathing exercises or meditation, can help alleviate pre-operative anxiety.
- Ensure a good night’s sleep before the surgery.
11. Post-operative Preparations:
- Set up the home for a comfortable recovery. This might include preparing meals in advance, setting up a comfortable resting spot with necessary items within arm’s reach, and ensuring a safe, slip-free environment.
In conclusion, while the thought of surgery can be daunting, being well-prepared can significantly ease the process. By following the pre-operative instructions closely and maintaining open communication with the healthcare team, patients can optimize their outcomes and recovery after gallbladder surgery.
Post-operative care
Recovering from gallbladder surgery, commonly known as cholecystectomy, requires careful attention to post-operative care to ensure optimal healing and to minimize complications. Here’s a comprehensive guide to the post-operative care recommendations:
1. Wound Care:
- Dressing: Keep the surgical dressing dry and intact for the first 48 hours unless otherwise advised by the surgeon.
- Showering: Typically, it’s okay to shower after 48 hours, but avoid soaking the wound (e.g., no baths, swimming, or hot tubs) until fully healed.
- Incision Monitoring: Regularly check the incision sites for signs of infection such as redness, warmth, increased swelling, or discharge.
2. Pain Management:
- Medication: The surgeon may prescribe pain relievers. Always use as directed and avoid over-the-counter pain medications without consulting the doctor.
- Alternative Methods: Gentle ice packs can reduce swelling and alleviate pain. However, always cover the ice pack with a cloth to protect the skin.
3. Physical Activity:
- Rest: Ensure adequate rest for the first few days post-surgery.
- Limited Activity: Refrain from heavy lifting (typically anything over 10 pounds) and strenuous activities for at least a week or as advised.
- Walking: Begin with short, frequent walks to promote blood circulation and gradually increase activity level.
4. Dietary Recommendations:
- Start Slow: Begin with clear liquids and gradually advance to solid foods.
- Low-Fat Diet: Initially, opt for a low-fat diet as the body adjusts to the absence of the gallbladder.
- Stay Hydrated: Drink plenty of water to help flush out anesthesia and to aid the healing process.
- Monitor for Digestive Issues: Some people may experience diarrhea or changes in bowel habits. If these persist, consult a doctor.
5. Follow-up Appointments:
- Ensure to attend all scheduled post-operative check-ups so the surgeon can monitor the healing process and address any concerns.
6. Monitoring for Complications:
- Be alert for signs of potential complications such as persistent nausea or vomiting, undue fatigue, yellowing of the skin or eyes (jaundice), dark urine, light-colored stools, or high fever. Seek medical attention if any of these symptoms arise.
7. Avoid Driving:
- Typically, avoid driving for at least a week or while taking narcotic pain medications.
8. Clothing:
- Wear loose, comfortable clothing that doesn’t press on the incision site.
9. Emotional Health:
- It’s not uncommon to feel a range of emotions after surgery. Communicate feelings with loved ones or consider professional counseling if feelings of anxiety or depression persist.
10. Medications:
- Before resuming regular medications, especially blood thinners or diabetes medications, consult with the healthcare provider.
11. Avoid Smoking:
- Smoking can impede the healing process. If possible, use the post-operative period as an opportunity to quit or reduce smoking.
12. Limit Alcohol Intake:
- Refrain from consuming alcohol, especially when taking pain medications.
13. Sexual Activity:
- While there’s no fixed rule, it’s generally advisable to wait at least a week or until the patient feels comfortable.
14. Returning to Work:
- Depending on the nature of the job and the type of surgery (open vs. laparoscopic), returning to work can vary. Typically, most people can return to work within a week or two, but those with more physically demanding jobs may require more time off.
In conclusion, the post-operative period after gallbladder surgery is a crucial time that requires attention, care, and patience. By adhering to the guidelines provided by the healthcare team and promptly addressing any concerning symptoms, patients can expect a smooth recovery journey.
Common physical sensations after surgery
Following gallbladder surgery, or cholecystectomy, patients often experience a variety of physical sensations. Some are a normal part of the healing process, while others can be a sign of potential complications. Here are the most commonly reported sensations after the procedure:
1. Pain:
- Incision Pain: Pain or discomfort around the surgical site is expected. For laparoscopic surgery, this might be in multiple smaller areas, while open surgery typically results in pain in a larger incision area.
- Shoulder Pain: Surprisingly to some, referred pain in the shoulder is common after laparoscopic cholecystectomy. This is due to the carbon dioxide used to inflate the abdomen, which can irritate the diaphragm and refer pain to the shoulder.
2. Bloating:
The abdomen might feel swollen or distended. This can also be attributed to the carbon dioxide gas used during the laparoscopic procedure.
3. Nausea or Vomiting:
Some patients might feel nauseated or even vomit post-surgery. This can be a side effect of anesthesia or pain medications.
4. Itching:
The incision sites can become itchy as they begin to heal. Additionally, some people might have an allergic reaction to surgical tapes or adhesives, which can intensify the itchiness.
5. Fatigue:
Feeling tired or drained is normal after any surgical procedure. The body is using energy to heal, and the effects of anesthesia can linger for a day or two.
6. Difficulty with Bowel Movements:
- Constipation: This is a common side effect of some pain medications and the disruption of normal eating and bowel routines due to surgery.
- Diarrhea: Some patients might experience changes in bowel habits, including diarrhea, after gallbladder removal, especially when consuming fatty foods.
7. Bruising:
It’s common to see some bruising around the incision sites or the surrounding area. This usually fades over a few days to weeks.
8. Muscle Weakness:
Especially in the first few days following surgery, patients might feel a lack of strength or stamina.
9. Loss of Appetite:
It’s not uncommon to have reduced appetite for several days after the surgery.
10. Tenderness:
The area around the surgical site might feel tender to touch.
11. Mild Fever:
A low-grade fever within the first 24 hours post-surgery might occur as the body responds to the surgical stress. However, a persistent or high fever could be a sign of an infection.
12. Changes in Urine and Stool:
Urine might appear darker than usual, and stools could be lighter in color in some cases.
13. Throat Discomfort:
If a breathing tube was used during the surgery, there might be a sensation of throat soreness or scratchiness.
It’s essential to remember that while many of these sensations are common and expected, any symptom that feels severe, persistent, or out of the ordinary should be promptly discussed with a healthcare professional. Always prioritize personal well-being and ensure timely communication with the surgical team during the recovery process.
Potential complications and their signs
While gallbladder surgery, or cholecystectomy, is generally considered safe, like all surgeries, there are potential complications. It’s essential to recognize the signs of these complications early for timely intervention:
1. Infection:
- Signs:
- Redness, swelling, warmth, or discharge at the incision site.
- Persistent fever or chills.
- Foul-smelling drainage from the incision.
2. Bile Leak:
Sometimes, bile can leak into the abdominal cavity.
- Signs:
- Severe abdominal pain.
- Yellowing of the skin and eyes (jaundice).
- Fever.
3. Bleeding:
- Signs:
- Excessive bruising or swelling around the incision site.
- Low blood pressure.
- Dizziness or fainting.
4. Injury to the Bile Duct:
This is a rare complication but can have serious implications.
- Signs:
- Jaundice.
- Pale stools and dark urine.
- Abdominal pain.
5. Injury to the Intestines, Bowel, or Blood Vessels:
- Signs:
- Severe abdominal pain.
- Signs of internal bleeding, like dizziness, rapid heartbeat, and low blood pressure.
6. Deep Vein Thrombosis (DVT):
Blood clots can form in the legs after surgery.
- Signs:
- Swelling in one leg.
- Pain or tenderness in the leg, especially when standing or walking.
- Warm skin in the area of the clot.
- Red or discolored skin.
7. Pulmonary Embolism:
A blood clot can break free and travel to the lungs.
- Signs:
- Sudden shortness of breath.
- Sharp chest pain.
- Rapid heartbeat.
- Coughing up blood.
8. Pancreatitis:
Inflammation of the pancreas.
- Signs:
- Abdominal pain that radiates to the back.
- Nausea and vomiting.
- Fever.
9. Retained Gallstones:
Occasionally, gallstones might be left behind and can cause issues.
- Signs:
- Abdominal pain.
- Jaundice.
- Fever.
10. Adverse Reactions to Anesthesia:
- Signs:
- Confusion or memory loss.
- Difficulty breathing or shortness of breath.
- Chest pain.
- Nausea or vomiting.
11. Hernia at the Incision Site:
- Signs:
- A visible bulge near the incision site.
- Discomfort or pain at the site, especially when coughing or lifting.
12. Postcholecystectomy Syndrome:
Some patients may continue to experience symptoms like abdominal pain and diarrhea after gallbladder removal.
- Signs:
- Ongoing abdominal discomfort or pain.
- Changes in bowel habits.
It’s important for patients to be vigilant after their surgery. If they notice any of these signs or symptoms, they should seek medical attention immediately. Early detection and treatment of complications can improve outcomes and prevent more serious health issues.
Importance of post-operative check-ups
A cholecystectomy, commonly referred to as a gallbladder surgery, is a procedure to remove the gallbladder. As with any surgery, post-operative check-ups play a pivotal role in ensuring a smooth and effective recovery. Here’s why these check-ups are particularly crucial for gallbladder surgery patients:
1. Monitoring Surgical Site Healing:
- The surgeon needs to inspect the incisions, especially in the case of laparoscopic cholecystectomy, to ensure they are healing properly and to watch for signs of infection, inflammation, or herniation.
2. Detecting Complications Early:
- While rare, complications such as bile leakage, injury to nearby structures like the bile duct, or infections can occur. Early detection through check-ups can prevent these issues from worsening.
3. Evaluating Digestive Changes:
- The gallbladder plays a role in bile storage and fat digestion. A post-operative check-up helps in discussing any dietary modifications or digestive concerns a patient might be facing after the operation.
4. Pain Management:
- Persistent or severe pain can be an indicator of complications. Regular check-ups allow the surgeon to adjust pain management strategies as needed.
5. Guidance on Activity Levels:
- Resuming normal activities, including lifting heavy objects, can be restricted after gallbladder surgery. A healthcare provider will give guidelines on when and how to safely get back to these tasks.
6. Addressing Patient Concerns:
- Patients may have various questions or symptoms they’re unsure of after the surgery. Post-operative check-ups provide an avenue to address these concerns promptly.
7. Liver Function Tests:
- In some cases, doctors might want to assess liver function after gallbladder surgery, given the organ’s close association with the gallbladder.
8. Dietary Recommendations:
- The absence of a gallbladder can affect how one’s body handles certain foods, especially fatty ones. A post-operative visit can involve dietary recommendations to help manage this change.
9. Assessment of Emotional Well-being:
- Any surgery can be stressful and can take a toll on mental health. Healthcare professionals can check in on the patient’s emotional well-being and offer support or referrals if needed.
10. Record Keeping:
- Keeping updated medical records ensures continuity of care. Post-operative check-ups after gallbladder surgery help in documenting the patient’s recovery progress.
11. Planning Further Treatment:
- In rare cases, if gallbladder surgery was performed due to gallbladder cancer, post-operative visits might involve discussions about further treatments or surveillance.
12. Education and Prevention:
- Post-operative visits provide an opportunity to educate patients about signs of potential complications, care of the surgical site, and necessary lifestyle or dietary changes.
In essence, post-operative check-ups after gallbladder surgery serve multiple crucial functions, from ensuring physical healing and addressing any complications to offering emotional support and guidance. They are an integral component of the surgical journey, ensuring that the patient achieves the best possible recovery and long-term health outcomes.
Digestive changes after surgery
The gallbladder is a small organ that stores bile, a digestive fluid produced by the liver. It helps in the digestion of fats by releasing bile into the small intestine when fatty foods are consumed. After gallbladder surgery or cholecystectomy, the gallbladder is removed, leading to some potential changes in the digestive process. Here’s a breakdown of these changes:
1. Altered Bile Flow:
- Before Surgery: The gallbladder stores and concentrates bile, releasing it in larger amounts when needed, especially after the consumption of a fatty meal.
- After Surgery: The liver continues to produce bile, but there’s no storage facility. Instead, bile continuously drips into the small intestine, regardless of food consumption.
2. Difficulty Digesting Fats:
- Due to the continuous, rather than regulated, release of bile, the body might not have enough bile to handle large amounts of fat at once. This can make it harder for some people to digest fatty foods, leading to diarrhea or bloating.
3. Frequent, Loose Stools:
- Some people might experience more frequent bowel movements or loose stools after gallbladder removal. This is often due to bile irritating the intestines.
4. Gas and Bloating:
- Changes in bile release can affect gut bacteria and digestion, leading to increased gas and bloating for some individuals.
5. Changes in Bowel Habits:
- Some individuals may develop “bile acid diarrhea” or “bile salt diarrhea,” where bile acid irritates the intestine, leading to diarrhea. On the other hand, some might experience constipation due to changes in gut motility.
6. Food Intolerances:
- After surgery, certain foods might be less tolerated than before, especially fatty, greasy, or spicy foods. Consuming these can result in diarrhea, gas, or stomach discomfort.
7. Acid Reflux or Heartburn:
- Some individuals may experience increased symptoms of gastroesophageal reflux disease (GERD) or heartburn. This can be due to changes in gastric emptying or the continuous flow of bile into the stomach.
8. Weight Changes:
- Some people might lose weight due to a decrease in food intake from digestive discomfort or consciously reducing fat in their diet. Others might gain weight if they replace fats with sugary or refined carbohydrate foods.
Recommendations for Managing Digestive Changes:
- Dietary Adjustments: Gradually introducing fats to assess tolerance, opting for smaller, more frequent meals, and avoiding very fatty or greasy foods can help.
- Fiber: Consuming soluble fiber can bind to bile acid, potentially reducing diarrhea. Foods like oats, apples, and carrots are good sources.
- Medications: In cases of severe diarrhea, medications that bind to bile acids, like cholestyramine, can be prescribed.
- Stay Hydrated: If experiencing diarrhea, it’s essential to drink plenty of fluids to stay hydrated.
- Probiotics: These can help in rebalancing gut bacteria, potentially alleviating some digestive symptoms.
- Monitoring: Keeping a food diary can help pinpoint which foods might be causing discomfort or digestive issues.
In conclusion, while many people do not experience significant changes in their digestion after gallbladder surgery, some do face challenges. It’s crucial to work closely with a healthcare professional to address and manage any digestive changes effectively.
Foods to avoid and why
After gallbladder surgery (cholecystectomy), the body can react differently to certain types of foods due to the altered bile flow. While the liver continues to produce bile, the absence of the gallbladder means bile is no longer stored and concentrated but drips continuously into the small intestine. This can affect the digestion of certain foods, especially fats. Here’s a list of foods that are commonly recommended to limit or avoid shortly after gallbladder surgery:
1. High-Fat Foods:
- Examples: Fried foods, fatty cuts of meat, bacon, sausages, oils, butter, full-fat dairy, fast food.
- Reason: Without the gallbladder to release a concentrated amount of bile on demand, digesting large amounts of fats can be challenging. Consuming high-fat foods might lead to diarrhea and bloating.
2. Spicy Foods:
- Examples: Hot peppers, curries, hot sauces.
- Reason: Spicy foods can irritate the digestive system, leading to discomfort, especially when the system is already sensitive post-surgery.
3. Dairy Products:
- Examples: Full-fat milk, cheese, ice cream, creams.
- Reason: Dairy can be hard to digest due to its fat content, and some people may also have a degree of lactose intolerance that can cause bloating, gas, and diarrhea.
4. Gas-Producing Foods:
- Examples: Beans, lentils, broccoli, cabbage, onions, cauliflower.
- Reason: While these foods are generally healthy, they can cause gas and bloating. After surgery, the digestive system might be more sensitive to these effects.
5. Caffeinated Beverages:
- Examples: Coffee, certain teas, some sodas.
- Reason: Caffeine can stimulate the digestive system and might cause diarrhea in some post-operative patients.
6. Sugary Foods:
- Examples: Pastries, candies, sugary drinks, and desserts.
- Reason: Sugary foods can exacerbate diarrhea in some people after gallbladder removal. Plus, excessive sugar consumption can lead to other health issues, like weight gain.
7. Processed Foods:
- Examples: Packaged snacks, chips, certain frozen meals.
- Reason: These foods often contain high amounts of unhealthy fats, sugars, and salt, making them harder to digest and potentially irritating to the digestive system.
8. Alcoholic Beverages:
- Reason: Alcohol can irritate the digestive system and may exacerbate symptoms like diarrhea or indigestion.
Recommendations:
It’s important to note that everyone’s body is different, and while some people might have a hard time with certain foods, others may tolerate them without issue. After surgery:
- Gradual Introduction: Start by eating small, frequent meals and slowly reintroduce foods to gauge how your body reacts.
- Listen to Your Body: If a particular food causes discomfort or digestive issues, it’s best to avoid it and then retry after some time.
- Seek Professional Advice: Always consult with a healthcare professional or nutritionist regarding any dietary changes, especially after surgery.
In conclusion, while the above foods might commonly cause issues after gallbladder surgery, it’s essential to maintain a balanced diet. Over time, many people can reintroduce these foods without problems as the body adapts to the absence of the gallbladder.
Building a balanced diet for optimal health
Following gallbladder surgery, or cholecystectomy, the body’s ability to digest certain foods, especially fats, may be affected. The gallbladder’s primary role was to store bile, which aids in fat digestion. Without it, bile flows directly into the intestines in smaller amounts, making fat digestion less efficient. Hence, dietary adjustments are often needed. Here’s how to build a balanced diet post-gallbladder surgery:
1. Gradual Introduction of Fats:
- Start Slow: Initially, it’s advisable to follow a low-fat diet and gradually introduce fats to determine tolerance.
- Healthy Fats: When reintroducing, focus on healthy fats like avocados, olive oil, nuts, and seeds. Monitor how your body responds.
2. Lean Proteins:
- Sources: Lean meats, poultry, fish, tofu, legumes, and eggs.
- Benefits: They provide essential amino acids without excessive fat, which can be beneficial in the early post-operative stages.
3. Whole Grains:
- Sources: Brown rice, quinoa, whole grain pasta, oats.
- Benefits: They offer sustained energy and are rich in fiber, which can aid in digestion and bowel regularity, especially if post-surgery constipation is an issue.
4. Hydration:
- Keeping well-hydrated is crucial, especially if diarrhea or loose stools become a problem after surgery.
- Aim for 8-10 glasses of water daily and include herbal teas or broth if desired.
5. Fiber-Rich Foods:
- Gradual Introduction: While fiber is essential, introduce it gradually to see how your digestive system reacts post-surgery.
- Sources: Fruits, vegetables, legumes, and whole grains.
6. Limit Spicy and Acidic Foods:
- Reason: These can irritate the digestive system, especially soon after surgery.
7. Limit Sugary Foods:
- High sugar foods might exacerbate diarrhea in some people post-surgery.
8. Small, Frequent Meals:
- Instead of three large meals, consider 5-6 smaller meals throughout the day. This can prevent overloading the digestive system and allow for better absorption of nutrients.
9. Limit Dairy Initially:
- Some people find dairy harder to digest after gallbladder removal, especially full-fat varieties. Monitor tolerance and consider lactose-free options if needed.
10. Mindful Eating:
- Pay close attention to how different foods affect your digestion. Keeping a food diary might be helpful in the initial stages.
11. Vitamins and Minerals:
- Ensure you’re getting a good spectrum of vitamins and minerals. If fatty fish is hard to digest, consider an omega-3 supplement. If you’re reducing dairy, ensure adequate calcium and vitamin D intake from other sources or supplements.
12. Professional Guidance:
- Consider seeking advice from a dietitian who can guide dietary choices based on individual needs post-surgery.
Tips:
- Flexibility: Everyone’s body is different. What works for one person post-surgery might not work for another. It’s essential to listen to your body and adjust accordingly.
- Avoid High-Fat Trigger Foods: These might include fried foods, rich desserts, and certain cuts of meat. Reintroduce them one at a time to gauge tolerance.
- Chew Thoroughly: This aids digestion and can help alleviate potential digestive discomfort.
How the liver compensates for the missing gallbladder
The gallbladder is a small organ situated beneath the liver, responsible for storing and concentrating bile, a digestive fluid produced by the liver. This bile helps in the emulsification and breakdown of dietary fats in the intestines. When the gallbladder is removed (a procedure called cholecystectomy), the body undergoes certain adaptive changes to manage bile flow and fat digestion. Here’s how the liver and digestive system compensate for the missing gallbladder:
1. Continuous Bile Flow:
- Before Removal: The gallbladder would store bile and release it in response to fatty meals, providing a concentrated burst of bile to help digest the fats.
- After Removal: Without the gallbladder, the liver continues to produce bile. However, instead of being stored and released in large amounts, bile is now released directly into the small intestine in a slow and continuous manner, regardless of the presence of food.
2. Decreased Bile Concentration:
- The bile that is directly secreted into the intestines is less concentrated than the bile that was stored in the gallbladder. While this diluted bile is still effective in aiding digestion, it may be less efficient at digesting large amounts of fat at once.
3. Digestive Adaptation:
- Over time, the digestive system tends to adjust to the new pattern of bile flow. Many individuals can eventually consume a normal diet, though some might still need to be cautious with very fatty meals to avoid digestive discomfort.
4. Increased Bile Storage in Bile Ducts:
- Some degree of bile storage might occur in the common bile duct and hepatic ducts. While they cannot store as much bile as the gallbladder, they can expand slightly in response to the liver’s bile production.
5. Alteration in Gut Microbiota:
- Some studies suggest that the absence of the gallbladder might lead to changes in the composition of gut bacteria. The significance and long-term impact of these changes are still being researched.
6. Dietary Adjustments:
- While not a physiological compensation by the liver, dietary modifications post-surgery can assist in complementing the continuous bile flow. Consuming smaller, more frequent meals and reducing high-fat foods can make it easier for the continuous, low-concentration bile flow to manage fat digestion.
7. Colon Adaptation:
- The colon might absorb some of the continuously dripping bile, especially during fasting periods. Over time, this can lead to changes in bowel habits for some individuals, such as increased frequency or urgency.
Key Takeaways:
The human body is remarkably adaptable. While the gallbladder plays a specific role in digestion, the body can adjust to its absence. The liver, intestines, and other parts of the digestive system work together to ensure dietary fats are still processed. Most people can lead a normal life post-gallbladder surgery, though individual experiences may vary, and dietary adjustments can help optimize digestive comfort.
The role of bile in digestion without a gallbladder
Bile is an essential digestive fluid produced by the liver that plays a vital role in the emulsification and breakdown of dietary fats. The gallbladder’s primary function is to store and concentrate this bile, releasing it into the small intestine in response to a meal, especially one that’s high in fat. However, when the gallbladder is removed, the process of bile release and its interaction with food changes. Here’s how bile functions in digestion without a gallbladder:
1. Continuous Bile Release:
- Before Removal: With a gallbladder, bile is stored and released in large, concentrated amounts in response to dietary fat entering the small intestine.
- After Removal: Without the gallbladder, the liver continues to produce bile, but it drips continuously in a less concentrated form directly into the small intestine, regardless of meal consumption.
2. Emulsification of Dietary Fats:
- Even without the gallbladder, bile still performs its primary function: emulsifying dietary fats. Emulsification is the process by which large fat globules are broken down into smaller droplets, increasing the surface area for digestive enzymes (lipases) to act upon. This process ensures the fats can be further digested and absorbed.
3. Digestive Efficiency:
- Due to the continuous and less concentrated nature of bile release post-gallbladder removal, the efficiency of fat digestion might be reduced, especially when consuming large, fatty meals. This is why some individuals experience digestive discomfort or changes in bowel habits after consuming foods high in fat.
4. Absorption of Fat-Soluble Vitamins:
- Bile plays a crucial role in the absorption of fat-soluble vitamins: A, D, E, and K. Even without the gallbladder, bile ensures that these vitamins, once extracted from food sources, are absorbed into the bloodstream from the intestines.
5. Neutralization of Stomach Acid:
- Bile, which is alkaline in nature, helps to neutralize the stomach acid that enters the small intestine, creating a more optimal pH for the enzymes in the intestine to function.
6. Excretion of Waste Products:
- Bile facilitates the excretion of waste products like bilirubin (a byproduct of old red blood cells) and excess cholesterol. These compounds are incorporated into the feces and expelled from the body.
Key Considerations:
Without a gallbladder, the dynamic of bile release changes, but the significance of bile in digestion remains crucial. The body typically adapts to this new pattern of bile release. However, individuals might need to make dietary adjustments, such as reducing the intake of large, fatty meals, to accommodate the continuous, less concentrated bile flow and ensure optimal digestion. Over time, many individuals find they can return to a relatively normal diet, though some may always need to be more mindful of their fat intake.
Dealing with potential digestive discomforts
After gallbladder surgery (cholecystectomy), many individuals experience changes in their digestion. This is due to the alteration in bile delivery to the small intestine. While the body often adapts over time, managing the initial digestive discomforts can improve the post-operative experience. Here are strategies and tips to deal with these potential discomforts:
1. Gradual Introduction of Fats:
- Initially, follow a low-fat diet. Slowly reintroduce fats into your meals to determine tolerance.
- Focus on healthy fats such as avocados, olive oil, nuts, and seeds, but be mindful of the quantities.
2. Eat Smaller, Frequent Meals:
- Consuming smaller portions spread throughout the day can prevent overloading the digestive system and can help with the continuous, less concentrated bile flow.
3. Limit High-Fat and Spicy Foods:
- Foods that are high in fat or overly spicy can exacerbate digestive discomforts. This includes fried foods, fatty cuts of meat, dairy products, and spicy dishes.
4. Increase Fiber Intake Gradually:
- Fiber can aid in normalizing bowel movements, but it’s essential to introduce it slowly to avoid excessive gas and bloating.
- Consider sources like whole grains, fruits, and vegetables, but be cautious with gas-producing foods like beans and certain vegetables such as broccoli and cauliflower initially.
5. Stay Hydrated:
- Drink plenty of water to support digestion and prevent constipation.
6. Limit Dairy Consumption:
- Some people find dairy harder to digest after gallbladder removal. If dairy causes discomfort, consider switching to lactose-free options or alternatives like almond or oat milk.
7. Avoid Sugary and Carbonated Beverages:
- These can exacerbate symptoms like bloating, gas, and diarrhea.
8. Keep a Food Diary:
- Track what you eat and any subsequent symptoms. This can help identify trigger foods that might be contributing to discomfort.
9. Over-the-counter (OTC) Remedies:
- Products like antacids or simethicone can help with minor symptoms. However, always consult with a healthcare professional before starting any medication.
10. Consider Probiotics:
- Probiotic supplements or foods like yogurt can help in maintaining a healthy gut microbiota balance, potentially reducing symptoms like bloating and diarrhea.
11. Engage in Regular Physical Activity:
- Gentle activities like walking can promote digestion and reduce feelings of bloating or discomfort.
12. Seek Professional Guidance:
- If digestive discomfort persists or is severe, it’s essential to seek advice from a gastroenterologist or a registered dietitian who can provide tailored recommendations.
13. Medications:
- In cases where diarrhea becomes chronic, medications such as cholestyramine can be prescribed to bind bile acids and provide relief.
Adapting to life after gallbladder surgery requires patience and a degree of trial and error to find what works best for your body. Over time, many individuals find a balance and return to a comfortable digestive routine. However, if symptoms persist or are severe, it’s essential to consult with healthcare professionals to ensure optimal recovery and health.
Busting myths related to gallbladder removal
Gallbladder removal, or cholecystectomy, is a common surgical procedure. As with many medical interventions, various myths surround it. Here, we’ll address and debunk some of the most common misconceptions about gallbladder removal.
Myth 1: You can’t digest fat without a gallbladder.
Truth: While the gallbladder does store bile to aid in fat digestion, you can still digest fat without it. The liver continues to produce bile post-surgery. Although bile is now released in a continuous and less concentrated manner into the small intestine, the body generally adjusts to handle fat digestion over time. Some individuals may need to moderate their fat intake initially, but most can consume a balanced diet after recovery.
Myth 2: Gallbladder removal guarantees no more abdominal pain.
Truth: While many people experience relief from gallstone-related pain after surgery, some might experience postcholecystectomy syndrome, which includes symptoms like abdominal pain and diarrhea. The reasons can vary, including bile duct injury or remaining gallstones. It’s crucial to consult a doctor if pain persists post-surgery.
Myth 3: Diet doesn’t matter after gallbladder removal.
Truth: While many people can resume a normal diet eventually, dietary modifications can help in the initial post-operative phase to prevent discomfort due to the altered bile flow. Avoiding large, fatty meals can help accommodate the continuous bile flow and ensure digestive comfort.
Myth 4: Gallbladder problems are solely due to diet.
Truth: While diet can contribute to gallstone formation and other gallbladder issues, factors like genetics, pregnancy, certain medical conditions, and medications also play a role.
Myth 5: Gallbladder removal affects longevity.
Truth: There is no scientific evidence to suggest that life expectancy is reduced after gallbladder removal. People can lead a healthy and normal life without a gallbladder.
Myth 6: Gallbladder surgery is always a major operation.
Truth: While open cholecystectomy is a more extensive procedure, most gallbladder removals today are performed laparoscopically, which is minimally invasive. Recovery from laparoscopic surgery is generally quicker with less post-operative discomfort.
Myth 7: Everyone will experience diarrhea after surgery.
Truth: While some individuals might experience diarrhea or changes in bowel habits due to continuous bile flow into the intestine, not everyone will. Over time, the body often adapts, and bowel habits normalize.
Myth 8: Gallstones can be dissolved or “flushed out” without surgery.
Truth: Some medications can dissolve cholesterol gallstones, but they can take months or years to work, are not always effective, and gallstones may recur. The so-called “gallbladder flushes” or “cleanses” promoted on some websites are not scientifically proven to be effective and could be harmful.
Key Points
Misinformation can lead to unnecessary fear or hesitation regarding medical decisions. If you or someone you know is contemplating gallbladder surgery or has concerns post-surgery, always consult with a healthcare professional to get accurate information and guidance.
How to address concerns and questions
Addressing concerns and questions about gallbladder surgery is crucial for patient comfort and understanding. Ensuring that patients are well-informed can help reduce anxiety, enhance cooperation, and improve post-surgical outcomes. Here’s a systematic way to address concerns:
1. Provide Informative Literature:
- Offer brochures or booklets detailing the cholecystectomy procedure, its benefits, and potential risks. This can serve as a reference for patients and their families.
2. Organize Pre-surgical Consultations:
- Schedule meetings with the surgical team or primary care physician to discuss the procedure in detail. Allow ample time for the patient to raise any concerns.
3. Encourage Open Communication:
- Encourage patients to list down their questions before the meeting. Assure them that no question is too trivial when it comes to their health.
4. Explain the Procedure:
- Describe the surgical method, whether it’s open or laparoscopic.
- Explain the reason for the surgery, the expected outcomes, and the potential risks.
5. Discuss Recovery:
- Provide a rough timeline for recovery.
- Discuss post-operative care, potential discomforts, dietary adjustments, and activity levels.
6. Address Dietary Concerns:
- Discuss potential digestive changes and the importance of diet in post-operative recovery.
- Offer dietary guidelines or refer the patient to a nutritionist if necessary.
7. Reassure on Common Misconceptions:
- Bust common myths about gallbladder removal, ensuring patients have accurate information.
8. Explore Alternatives and Limitations:
- While surgery might be the best option, discuss any alternatives available, their efficacy, and potential limitations.
9. Talk About Anesthesia:
- Explain the type of anesthesia that will be used and its risks. Discuss any previous experiences the patient might have had with anesthesia and address any related concerns.
10. Discuss Financial Aspects:
- If relevant, discuss the cost of the surgery, insurance coverage, and any out-of-pocket expenses.
11. Provide Emotional Support:
- Recognize and address the emotional aspects of undergoing surgery. If necessary, refer patients to counselors or support groups.
12. Encourage Second Opinions:
- If the patient is hesitant, suggest getting a second opinion. This can provide additional reassurance.
13. Post-operative Follow-up:
- Ensure the patient understands the importance of post-operative check-ups and adhering to medical advice during the recovery period.
14. Provide Contact Details:
- Offer a direct line of communication for any immediate concerns or questions. Knowing they can easily reach out to a healthcare professional can be reassuring.
So
Open, honest, and empathetic communication is the key to addressing concerns about gallbladder surgery. By providing clear information, being available for questions, and ensuring patients feel heard and understood, healthcare professionals can make the surgical experience less daunting and more manageable for those in their care.
Separating fact from fiction
Gallbladder surgery, or cholecystectomy, is one of the most commonly performed surgeries. However, like many medical procedures, myths and misconceptions surround it. Let’s separate fact from fiction:
1. “You can’t digest fats without a gallbladder.”
- Fact: You can still digest fats after gallbladder removal. The liver continues to produce bile, which aids in fat digestion. However, since bile is released continuously rather than in response to a meal, some individuals may need to adjust their fat intake initially.
2. “Diet doesn’t matter after gallbladder removal.”
- Fact: Dietary modifications, especially in the initial post-operative phase, can be beneficial. Consuming smaller, frequent meals and avoiding high-fat or spicy foods can prevent discomfort due to altered bile flow.
3. “All gallbladder surgeries are major operations with a long recovery time.”
- Fact: Most cholecystectomies are performed laparoscopically, which is minimally invasive. Laparoscopic surgeries often have a faster recovery time compared to open surgeries.
4. “You’ll never experience abdominal pain again after gallbladder removal.”
- Fact: While many experience relief from gallstone-related pain, some might have postcholecystectomy syndrome. This can result in symptoms like abdominal pain or diarrhea. Several factors, including bile duct issues, can be the cause.
5. “Gallstones can be easily dissolved or ‘flushed out’ without surgery.”
- Fact: Some medications can dissolve certain types of gallstones, but they may not always be effective, and recurrence is common. “Gallbladder flushes” or “cleanses” are not scientifically supported and could be harmful.
6. “You’ll automatically lose weight after gallbladder surgery.”
- Fact: Weight loss isn’t a direct result of gallbladder removal. Some people might lose weight initially due to dietary changes, but it’s not guaranteed.
7. “Everyone suffers from chronic diarrhea after gallbladder surgery.”
- Fact: While some individuals experience changes in bowel habits, not everyone will have chronic diarrhea. Many people’s bowel habits normalize over time.
8. “Gallbladder problems only arise due to a poor diet.”
- Fact: Diet can contribute to gallstone formation, but other factors like genetics, gender, age, pregnancy, certain medical conditions, and medications also play significant roles.
9. “If you don’t have gallbladder pain, you don’t need surgery.”
- Fact: Asymptomatic gallstones are common. While they don’t always require removal, in some cases, surgery may be recommended to prevent future complications.
10. “Gallbladder removal affects fertility and pregnancy.”
- Fact: Gallbladder surgery does not directly impact fertility. However, gallbladder issues can arise during pregnancy due to hormonal changes. If gallstones are present before pregnancy, a doctor might discuss potential risks and benefits of surgery.
When considering any medical procedure, it’s essential to base decisions on accurate information. Patients should consult with healthcare professionals to address concerns and obtain reliable information regarding gallbladder surgery.
Recommended Resources
List of helpful books, websites, and organizations
a list of helpful resources, including books, websites, and organizations, that provide information about gallbladder surgery and related topics:
Books:
- “The Gallbladder Survival Guide: How to Live a Normal Life with a Missing or Dysfunctional Gallbladder” by J. Bernal.
- “Gallbladder Removal: A Simple Guide To Gallstones And Gallbladder Diseases” by Kenneth Kee.
- “Eating Well After Gallbladder Surgery” by Cat Morrow.
- “Living Well Without a Gallbladder: A Guide to Postcholecystectomy Syndrome” by Brooke Keefer.
Websites:
- Mayo Clinic: This well-respected institution provides comprehensive information about gallbladder surgery, including risks, benefits, and recovery.
- WebMD: A widely recognized health website offering information on various topics, including cholecystectomy.
- MedlinePlus: An online health information resource, sponsored by the National Institutes of Health.
- Cleveland Clinic: Another reputable medical institution offering detailed information on gallbladder surgeries.
Organizations:
- American College of Gastroenterology (ACG): Offers resources for patients and professionals about various gastrointestinal diseases, including gallbladder conditions.
- American Gastroenterological Association (AGA): Provides guidelines, research, and patient resources related to gastrointestinal disorders.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Provides a wealth of resources on gallstones and gallbladder surgery.
- The International Hepato-Pancreato-Biliary Association (IHPBA): An organization that fosters learning and research on diseases and surgeries of the liver, pancreas, and biliary tract, including the gallbladder.
Remember, while these resources provide a wealth of information, it’s always crucial to consult with healthcare professionals when considering surgery or when looking for specific medical advice.
Disclaimer:
- “The information contained in this article is purely educational and is not intended to replace professional medical advice. Always consult with a healthcare specialist before undergoing any medical procedure.”